How is Access To Medicines a Human Rights Issue?
What is access to medicines?
In 2015, the international community adopted the Sustainable Development Goals (SDGs), a set of 17 goals to be achieved by 2030. Goal 3—which committed to “ensure healthy lives and promote well-being for all at all ages”—proposed a range of targets from addressing non-communicable diseases to substance abuse to environmental health. Imbedded in the fulfilment of Goal 3 was the target to end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases, and to combat hepatitis, water-borne diseases, and other communicable diseases. Goal 3 also called for the achievement of universal health coverage, greater investment in research and development of medicines for communicable and noncommunicable diseases, and as this chapter of the Health and Human Rights Resource Guide will discuss, the provision of access to affordable essential medicines.
What are essential medicines? By definition, essential medicines are those medicines that “satisfy the priority healthcare needs of the population,” and according to the World Health Organization (WHO), are selected on the basis of their estimated current and future public health relevance, evidence of efficacy and safety, and comparative cost-effectiveness. Medicines that meet these principles are published in the WHO’s model list of essential medicines, an inventory updated every two years and tailored to national or regional health needs in a national essential medicines list (EML). Countries can use national lists as a tool to prioritize their most pressing public health needs by focusing on public sector procurement and treatment of a limited and high-priority set of medicines.
Advances in scientific and technological innovation over the past several decades have changed the current picture of the world’s access to medicines. Innovation has motivated the development of new vaccines, reduced the prevalence of infectious diseases (for instance, polio and human papillomavirus),[1] and significantly decreased the global disease burden of HIV/AIDS. The invention of molecularly targeted therapies has even showed early promise for treating cancer, and the biomedical industry has made strides in strengthening the prevention, treatment, and control of transmissible and non-transmissible diseases.[2] Tuberculosis is illustrative of this progress: Between 1990 and 2013, the tuberculosis mortality rate fell by 45 percent, and the prevalence rate fell by 41 percent.[3]
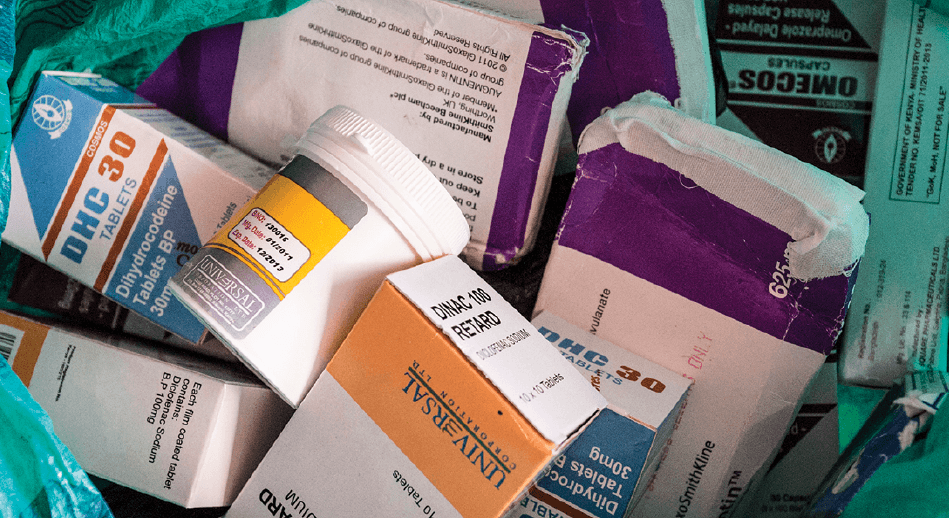
Despite notable progress, approximately 2 billion people around the world still face tremendous obstacles in accessing the medicines they need.[4] Moreover, the current research and development (R&D) model, which is largely market driven, is ill-equipped to address these gaps. It also should be noted that now more than ever, the high pricing of essential medicines is increasingly understood as a global problem affecting all countries, not just developing ones. While in the late nineties, the HIV/AIDS epidemic was the hallmark example of access problems, this picture has changed (prices of ARVs have come down to close to marginal cost of production in most countries, and at the end of 2014, 13.6 million people were able to access antiretroviral therapy[5],[6]), and the prevailing R&D model has us ill-prepared to respond to emerging infectious diseases such as Zika and Ebola; to neglected tropical diseases (NTDs) that predominantly affect populations with little purchasing power;[7] and to neglected populations, such as people living with rare diseases and children. The human rights-based approach put forth by this chapter will provide recommendations to resolve this incoherence between innovation and access by realigning global public health priorities and global health technology innovation.
This chapter intends to develop the current understanding of a human rights-based approach to access to medicines: it outlines the challenges that many populations face in accessing medicines (Section 1, part I), explains what understanding access to medicines through a human-rights based lens means (part II), summarizes human rights elements necessary for the realization of access to medicines (part III), and examines the tension between intellectual property (IP) rights and international human rights commitments (part IV). Part V focuses on key populations that encounter specific challenges within the broad landscape of enabling access to medicines, and Part VI recommends rights-based interventions and practices. After a tabular overview of the most relevant international and regional human rights standards related to the topic (Section 2), Section 3 discusses relevant human rights-based approaches to advocacy, litigation, and programming. Section 4 highlights specific country examples that have been successful in advancing the right to health and access to medicines for all, and the final section offers a glossary for further reading.
What are the issues and how are they human rights issues?
1. An overview of the international human rights framework
Access to essential medicines, nested in the right to the highest attainable standard of health, is well founded in international law. The 1946 Constitution of the World Health Organization and the 1948 Universal Declaration of Human Rights (UDHR) both expressly recognize the right to health. The 1966 International Covenant on Economic, Social, and Cultural Rights (ICESCR), which has 164 states parties, elaborates that the right to health includes “access to health facilities, goods, and services.” In General Comment 14 (2000) on the right to health, the Committee on Economic, Social and Cultural Rights (CESCR) interprets the normative content of article 12 of the ICESCR.[8] Although the ICESCR only requires the progressive realization of the right to health in the context of limited resources, there is a core set of minimum obligations which are not subject to progressive realization, including access to essential medicines.[9] The WHO, numerous national court cases and resolutions of the Human Rights Council, and the Doha Declaration on TRIPS and Public Health reaffirm access to essential medicines as a human right that must be available “for all.”
While states hold the core responsibility for essential medicines provision, these responsibilities are shared with other non-state actors. For example, pharmaceutical companies have human rights responsibilities described by the former UN Special Rapporteur on the Right to Health, including the duty to take all reasonable measures to make new medicines “as available as possible” for those in need.[10] Additionally, the UN Guiding Principles on Business and Human Rights, which were unanimously endorsed by the UN Human Rights Council in 2011, obliges the private sector to take responsibility for violations of human rights related to access to medicines.[11] The international community also has human rights obligations to assist governments lacking resources to achieve their minimum core duties through international cooperation and assistance.[12] In the face of disaster, the international community bears the duty to contribute to relief and humanitarian assistance by providing medical supplies as a matter of priority.[13]
2. What does a human rights-based approach (HRBA) contribute to access to medicines?
What does a human rights-based approach (HRBA) contribute to access to medicines? A HRBA identifies all human beings as having indivisible, interrelated rights, and in this case, to health and to access essential medicines. In addition to duties and entitlements, and as articulated by the WHO[14] and CESCR,[15] a HRBA applies the principles of non-discrimination and equality; participation and inclusion; accountability; and the rule of law to universal access policies.[16] These principles are conceived to inform all stages of programming and advocacy work, including monitoring and evaluation. A HRBA to access to medicines draws special attention to marginalized, disadvantaged, and excluded populations and endows all populations with the ability to achieve outcomes through an inclusive, transparent, and responsive process.[17],[18]
A human rights-based approach can also be applied to improve access to medicines at the policy level. The right to health offers a framework from which national health policies and laws can be shaped for universal and equitable access. The result can manifest as positive health outcomes and the individual realization of health rights and access to medicines. For instance, domestic constitutions that recognize access to medicines as part of the right to health can support individual claims for essential medicines in national courts.[19] A good example of this is documented in the final section of this chapter, where the right to health ratified by the Kenyan Constitution played a role in supporting litigation that ultimately advanced access to ARVs for people living with and affected by HIV and AIDS.
For individuals and communities living in relative poverty, recasting their lack of access to health care and essential medicines not as a failure of government policy, but as a denial of their rights, is tremendously empowering. When the needs essential to a life lived in dignity are elevated to the rank of legal entitlements, they have the power to change political discourse and the horizon of social expectations.[20] Reframing health as a human right is not simply to appear in court; it is to expand the bounds of what is possible, to mobilize neglected communities, to raise public awareness and trigger activism and education.
Importantly, application of the human rights framework also provides a clear delineation of the spheres of responsibility of different stakeholders, as circumscribed by human rights treaties, guiding principles, and general comments. States are obliged under international human rights law to respect, protect, and fulfill the right to health, which includes an obligation to adopt legislative, administrative, and budgetary measures to facilitate access to medicines that are affordable, accessible, culturally acceptable, and of good quality.[21] This obligation for a state to “use all available resources at its disposal” [22] to satisfy its obligations with respect to health will often require a state to make full use of the public health flexibilities available under international law.[23]
Meanwhile, pharmaceutical companies bear a responsibility to respect human rights vis-à-vis the Ruggie trinity of protect, respect, and remedy.[24] Within this framework, corporations have a duty to (a) avoid causing or contributing to adverse human rights impacts through their own activities, and address such impacts when they occur; and (b) prevent or mitigate adverse human rights impacts that are directly linked to their operations, products, or services by their business relationships, even if they have not contributed to those impacts.[25] Essentially, pharmaceutical firms bear a responsibility to act with due diligence to avoid infringing on the right to health. These responsibilities come into stark relief when pharmaceutical firms prioritize the enforcement of their intellectual property rights at the expense of their right-to-health obligations.
3. Human rights elements for access to medicines
According to General Comment 14, realizing the right to access medicines is contingent upon the realization of four interrelated elements. Medicines must be (1) available, (2) accessible (with accessibility implying affordability, physical accessibility, and accessibility of information), (3) acceptable, and (4) of good quality.[26]
In complement to the “AAAQ” framework described above, WHO has outlined the following four key building blocks as essential toward ensuring access to medicines in national health systems:
-
Rational selection and use of essential medicines, based on national lists of essential medicines and treatment guidelines;
-
Affordable prices for governments, health care providers and individuals;
-
Fair and sustainable financing of essential medicines as part of the national health care system through adequate funding levels and equitable prepayments systems, to ensure that the poor are not disproportionately affected by medicine prices; and
-
Reliable health and supply systems to ensure sufficient and a locally appropriate combination of public and private service providers.”[27]
Article 2 (1) of the ICESCR also calls for the “progressive realization” of economic and social rights. In other words, the ICESCR recognizes that some states are burdened by resource constraints, and therefore, allows obligations to be realized over time. Therefore, in theory, a lack of resources can justify non-compliance. However, as it was just mentioned and as the Limburg Principles on the Implementation of the International Covenant on Economic, Social and Cultural Rights have elaborated, the progressive realization of rights also suggests that states, regardless of their level of economic development, are obligated to take measures immediately and “move as expeditiously as possible” towards the realization of those rights.[28] Within the context of medicines, states must create and implement a reasonable action program to continuously improve access to essential medicines. State responsibility to provide essential medicines should be recognized in domestic law and given priority for public financing through sufficient budget allocation. Laws and policies within the health system (i.e. for universal health coverage or medicines pricing) and the broader legal order (i.e. for trade or intellectual property protection) should be aligned with achieving universal access to essential medicines. For instance, governments should make full use of the trade options under TRIPS flexibilities to safeguard access to essential medicines. (For an introduction on the TRIP Agreement and TRIPS flexibilities, see page 1-13.)
Regional instruments and documents agreed upon by the health community also clearly recognize the right to health. The African Charter on Human and Peoples’ Rights (art. 16), the European Social Charter (art. 11), the Protocol of San Salvador (art. 10),[29] the WHO Constitution,[30] the Ottawa Charter for Health Promotion,[31] and the Bangkok Charter for Health Promotion in a Globalized World[32] all consider health a fundamental human right.[33] These agreements can support access to medicines claims in domestic courts. In addition, the 1978 Declaration of Alma-Ata establishes a clear and important link between the provision of primary health care and the provision of essential drugs.[34]
International law gives clear guidance to states, and their implementation should be monitored in practice. Although more than 30 countries have not ratified the ICESCR, most states are party to at least one human rights instrument that recognizes the right to health. In terms of recognition in domestic law, 105 national constitutions include a degree of protection of the right to public health or medical care, while only 13 constitutions include the access to medicines as part of the right to health.[35],[36]
1. Intellectual property protection and trade
In addition to governments, non-state actors, such as pharmaceutical companies, have human rights responsibilities with respect to health. As explained by the UN Special Rapporteur on the right to health, Paul Hunt, pharmaceutical companies have the duty to take all reasonable steps to make a medicine “as accessible as possible” after it has been marketed, including to those who cannot afford (high) prices. These steps should be taken within a “viable business model.” [37] Paul Hunt contends that a company may be in breach of its responsibilities under the right to health “if a patent is worked without these steps being taken.”[38]
Even so, expanding economic globalization has tended to position the protection and enforcement of intellectual property (IP) rights at odds with international human rights law, and incoherencies have arisen between “patents” and “patients.” In 2015, the United Nations Secretary-General Ban Ki-moon recognized this tension when he established the UN High-Level Panel on Access to Medicines with a mandate to address the misalignment between the rights of inventors, international human rights law, trade rules, and public health. The culminating report posited that market-based models, which incentivize innovation, often lead to “insufficient investment… in R&D for diseases that predominantly affect the poor” and “prices charged by some right holders place severe burdens on health systems and individual patients, in wealthy and resource-constrained countries alike.”[39]
Among several recommendations, the report encouraged countries to reinforce the use of compulsory licenses through national laws, treat TRIPS flexibilities as a fundamental part of the TRIPS Agreement (not as an exception), and engage transparently in priority setting and coordination to prevent and stymie infectious diseases. (Compulsory licensing, the TRIPS Agreement.) It also encouraged the use of delinkage, a concept that refers to “delinking” the costs of R&D from the end prices of health technologies.
Patents
Pharmaceutical companies apply for patents for new, useful, and non-obvious inventions.[40] The public disclosure of an invention is rewarded with a twenty-year monopoly on its production, sale, and distribution. While pharmaceutical companies, and even governments, often claim that patents encourage innovation and provide crucial recuperation for research and development costs, the lack of transparency of R&D expenditure by the industry makes it almost impossible to determine the true costs of medicines.[41] Moreover, data has shown that the patent system tends to disproportionately benefit the holders of patent rights in developed countries at the cost of patients who consume technologies and goods in developing countries.[42],[43]
A patent confers so-called “negative rights” that allow the patent holder to exclude others from using his/her invention. Granted by the state, patents allow companies to control the production, distribution, use by others, and importation, and therefore, the price, of the product in question. Monopoly market power often leads to excessive prices and restricted access to affordable treatments for populations in developing and developed countries.[44],[45] Increasingly, new essential medicines are priced out-of-reach of patients in high-income countries as well.[46]
The purpose of the patent system is to incentivize innovation by giving the patentee exclusive monopoly rights over the use of the patented technology for a limited period of time, in return for disclosing valuable knowledge to society. The social gains derived from this system of protection must always be weighed against the inefficiencies resulting from monopoly market power and its vulnerability to abuse. Striking the optimal balance between innovation and access is extremely complex and inevitably influenced by the socioeconomic development agenda of the particular territory in which patent rights are enjoyed.
The patent regime’s vulnerability to abuse, particularly with respect to medicines treating for serious conditions – like hepatitis C or cancer – can be a matter of life or death.[47] As a UN expert consultant on access to medicines has written,
“While intellectual property rights have the important function of providing incentives for innovation, they can, in some cases, obstruct access by pushing up the price of medicines. The right to health requires a company that holds a patent on a lifesaving medicine to make use of all the arrangements at its disposal to render the medicine accessible to all.”[48]
The use of patent monopolies to limit generic competition compromises the “accessibility” (through affordability) of medicines, an issue that has been hotly debated in many countries. For example, in South Africa, the use of patents to block access to low-cost generic medicines have historically been responsible for high-priced essential medicines for HIV/AIDS and cancer, denying access to life-saving treatment for many. Similar strategies to challenge patent rights have been initiated in other developing countries. For example, in India, a patent application for Lopinavir/ritonavir (a treatment for HIV) manufactured by Abbott Laboratories (now AbbVie), was refused after I-MAK, a U.S.-based not-for-profit, filed a pre-grant opposition to it. I-MAK claimed that Abbott’s drug fell under Article 3(d) of the Indian patent law, which states “the mere discovery of a new form of a known substance which does not result in the enhancement of the known efficacy of that substance or the mere discovery of any new property or new use for a known substance or of the mere use of a known process, machine or apparatus unless such known process results in a new product or employs at least one new reactant.” I-MAK concluded that had Abbott secured a patent over a “new” formulation of Lopinavir/ritonavir, treatment for HIV/AIDS would have become out of reach for many. I-MAK’s litigation and advocacy work is highlighted in the best practices section (Section IV) of this chapter.
It is important to reverse the commonly held assumption that patent monopolies are the only means of recuperating the costs of, and therefore incentivizing, research and development for much-needed health technologies. While R&D is in fact needed to develop new drugs, a significant portion of this pivotal research is conducted with public financing. For example, advocates have pointed out that many antiretrovirals (anti-HIV drugs) were developed in public-funded laboratories.[49] Sofosbuvir, the high cost and highly effective drug for Hepatitis C, was also developed with public funding. Moreover, robust reports and analyses have also debunked the notion that patents are needed to recoup R&D costs.[50] A report by the Commission on Intellectual Property Rights, Innovation and Public Health finds, “…[W]here the market has very limited purchasing power, as is the case for diseases affecting millions of poor people in developing countries, patents are not a relevant factor or effective in stimulating R&D and bringing new products to market.”[51]
The introduction of the 1980 Bayh-Dole Act in the United States catalyzed significant research by allowing universities and public research institutions to patent the products of federally-funded research. However, limiting access to such discoveries through patent monopolies forces taxpayers to pay twice for the benefits of publicly-funded research.[52] The provision of public funding for research and development should instead be conditioned on strong, enforceable policies with respect to data sharing, open access publishing, non-exclusive licensing, participation in public sector patent pools, and affordability for low-income populations.[53]
Unfortunately, R&D shortfalls are most pronounced in developing countries where high-priority diseases are concentrated. Since pharmaceutical companies use patents to prevent competition, they are able to retain monopoly pricing on their drugs, making purchasing them nearly impossible for patients who—many lacking health insurance—must pay out of pocket for these life-saving medicines.[54]
The TRIPS Agreement
The Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) came into force in January 1995 in response to the growing need for multilateral cooperation on the regulation of intellectual property (IP). Developed by the World Trade Organization (WTO), the TRIPS Agreement globalized intellectual property requirements for the first time and marked a change in the way countries around the world interacted with the patent system. Prior to the establishment of TRIPS, intellectual property was regulated from country to country. Governments were able to tailor laws, policies, and practices to meet national priorities, and in some cases, excluded pharmaceuticals from patent protection altogether in order to safeguard the public’s health. Describing an age before the TRIPS Agreement, Ellen ‘T Hoen wrote, “The patenting of essential goods such as medicines and foods was long considered an act against the public interest.”[55]
New provisions embedded within TRIPS required WTO members to provide patents for all new, non-obvious, and useful inventions for at least 20 years (excluding the least developed countries and a few non-WTO Members, such as Somalia).[56]
Because patentability criteria are established by states and not by the WTO, states have significant discretion to define the parameters of patentability in a manner reflective of their domestic public health needs. For example, a developing country may decide to apply rigorous patentability criteria to ensure that generic firms are not unreasonably excluded from the market by incumbents who seek follow-on patents for new uses of known substances.[57] Striking the optimal balance between innovation and access will inevitably require a consideration of both public health needs and the domestic socio-economic landscape. Overly stringent patentability criteria also has the potential to discourage investment by foreign firms who fear that their intellectual property may not be adequately protected, thereby potentially jeopardizing economic development plans.
The DOHA Declaration
In November 2001 in Doha, Qatar, negotiations took place at the fourth WTO ministerial conference to address the TRIPS Agreement and the misalignment between profit-driven innovation models and public health. The result was the adoption of the Doha Declaration, a separate declaration on TRIPS and public health designed to respond to concerns about the implications of the TRIPS Agreement for access to medicines.
The declaration clarified that the TRIPS Agreement “does not and should not prevent member governments from acting to protect public health.” It also emphasized governments’ right to use TRIPS “flexibilities,” which are safeguards imbedded within the TRIPS Agreement that enable countries to adopt provisions to ameliorate the impact of patents on their population’s public health. Acknowledging “the seriousness of the concerns expressed by the least-developed countries (LDCs),” the declaration allowed these countries not to grant or enforce pharmaceutical product patents until at least 2016.[58] Paragraph 4 powerfully states, “[W]hile reiterating our commitment to the TRIPS Agreement, we affirm that the Agreement can and should be interpreted and implemented in a manner supportive of WTO Members’ right to protect public health and, in particular, to promote access to medicines for all.”[59]
To ensure strong IPR protection does not impede access to essential medicines, the declaration clarifies the scope of certain safeguards for all WTO members, which are embodied within the TRIPS Agreement. For instance, the declaration clarified that countries can determine the grounds upon which they issue compulsory licences for the generic manufacture of patented drugs.[60] The Doha Declaration also recognized the rights of governments to choose their own regime for parallel importation. Parallel imports are authentic products sold under intellectual property protection (copyright, patent, or trademark) in one country and shipped to another country without the manufacturer’s permission.[61] In the pharmaceutical context, parallel imports are genuine goods produced under patent, placed into circulation in one geographic market, and then imported into a second geographical market without the patentee’s authorization.[62] The legality of parallel imports depends on the choice of territorial exhaustion of the patent holder’s rights: national exhaustion means that rights are exhausted upon first sale within a nation but patent owners may prohibit parallel imports from abroad; regional exhaustion permits parallel imports among member countries (for example, within the European Union) but not from outside the region; and international exhaustion permits parallel imports from anywhere in the world as the patent holder’s rights are considered to be exhausted upon first sale in any country.[63] Typically, parallel importation is utilized to obtain drugs at their lowest price by exploiting price differences between markets. The Doha Declaration affirmed that countries are free to establish their own regime for parallel importation without challenge.[64]
Finally, the Doha Declaration waived the obligation of least developed country members (LDCs) to provide patent protection for pharmaceutical inventions until January 1, 2016, a deadline which has now been extended to January 1, 2033.[65] LDCs are also not required to provide patent protection to any invention at all until July 1, 2021, or until such a date on which they cease to be a least developed country member, whichever date is earlier.[66]
The Doha Declaration clarified that priorities under international trade law and international human rights law should be conversant with one another.[67] However, the promise of the Doha Declaration, which sought to protect the public’s health, has recently come under threat as states engaged in trade negotiations are pressured by governments and pharmaceutical companies alike to adopt even stricter conditions in their patent laws. These conditions are known as “TRIPS-plus” provisions because they require stricter protection of intellectual property than is required by the TRIPS Agreement. (Stricter conditions put binding obligations on countries to implement certain IP provisions beyond what is required by TRIPS.) Included among these strategies are preventing generic producers from using clinical data from the patented medicine to enter the market (data exclusivity),[68] and so-called patent “evergreening,” the practice of applying for multiple, successive patents on minor or insignificant variants or indications of already-patented compounds to extend the period of market exclusivity. While individual countries are free to implement strict patentability criteria that would prevent or limit evergreening, TRIPS-plus provisions, such as the obligation to grant patents for second medical use, would further facilitate the patenting of non-genuine innovations, or “evergreening.” Both processes extend companies’ monopolies, often prolonging high prices on medicines. An example of an attempt to “evergreen,” employed by Abbott Laboratories, is highlighted in Section 4 of this chapter. I-MAK filed a pre-grant opposition in response, as a result of which the patent was not granted. The UN Secretary-General’s High Level Panel on Access to Medicines explicitly recommended that WTO members make full use of the policy space available in TRIPS Article 27 by adopting and applying rigorous definitions of invention and patentability to curtail evergreening and ensure that patents are awarded only for genuine innovations.[69]
Although the Doha Declaration encouraged greater use of the public health flexibilities available under TRIPS, some countries have been unable or unwilling to make greater use of them. To address this failing, several public interest organizations – CEHURD in Uganda is one example – have intervened. In a policy brief, CEHURD encouraged the Ugandan government to maximize public health benefits from the new IPR protection regime by “making the most” of all flexibilities within TRIPS and adopting only the minimum levels of IPR protection that the agreement requires. A case study outlining this work is highlighted at the end of this chapter (Section 4). Additionally, international and multilateral institutions, including the United Nations Development Programme (UNDP), WHO, UNITAID, and the Global Fund, have strongly supported and encouraged the use of TRIPS flexibilities. For instance, in 2016, UNITAID adopted a resolution on the use of the intellectual property flexibilities enshrined in the global trading system allowing developing countries to facilitate access to affordable medicines.[70]
In addition, free trade agreements (FTAs) and investment treaties between states seek to build even stricter IP regimes that exceed the minimum provisions in the TRIPS Agreement through the inclusion of TRIPS-plus provisions.[71] The United States, a principal exporter of intellectual property, has negotiated FTA agreements with Thailand, South Korea, Singapore and many other governments to increase the longevity of protection on patented drugs.[72] TRIPS-plus provisions threaten to overshadow the utilization of public health safeguards to protect public health by, inter alia, requiring patents for new uses of known substances, prohibiting pre-grant opposition, imposing data exclusivity periods, extending patent terms beyond twenty years for regulatory or marketing delays, and imposing restrictions on compulsory licensing and parallel imports.[73],[74] The 2009 Report of the Special Rapporteur on the right to health, Anand Grover, explicitly cautioned against the inclusion of TRIPS-plus provisions in international trade and investment treaties, emphasizing that such agreements “have had an adverse impact on prices and availability of medicines, making it difficult for countries to comply with their obligations to respect, protect, and fulfil the right to health.”[75] The Special Rapporteur recommended that developing countries and LDCs “not introduce TRIPS-plus standards in their national laws” and that developed countries “not encourage developing countries and LDCs to enter into TRIPS-plus FTAs and … be mindful of actions which may infringe upon the right to health.”[76] The UN Secretary General’s High-Level Panel on Access to Medicines echoed these calls, recommending that “[g]overnments engaged in bilateral and regional trade and investment treaties should ensure that these agreements do not include provisions that interfere with their obligations to fulfil the right to health” and that governments conduct public health impact assessments prior to entering into such agreements.[77]
Research and Development
The current innovation model primarily relies on market monopolies and high prices to fund research and develop new medicines. Describing the “prevailing model,” the aforementioned UNHLP report summarized: “[T]he biomedical industry, with the help of well-established intellectual property protection mechanisms, test data exclusivity, and significant public funding of research, invests in R&D, obtains marketing approval and pays for related expenses by charging prices that allow them to recover these substantial costs and generate a profit. Shareholders who invest in biomedical companies do so with the expectation of generating a return on investment.”[78] This model results in several perverse incentives for R&D and prioritizes the development of treatments for profitable diseases affecting the affluent while often neglecting the needs of the poor and marginalized who are unable to pay high end-product prices. The effects of the R&D model are also felt globally and regardless of socioeconomic status. For instance, antimicrobial resistance (AMR) represents a growing global health threat, and yet, since the development of effective antibiotics is both expensive and unprofitable, the market-driven R&D system has little incentive to respond. The existing drug development paradigm requires high levels of antibiotic use in order to recover the costs of R&D, but mitigating the spread of antimicrobial resistance demands just the opposite: severe restrictions on distribution and use.[79] As a result, R&D remains woefully inadequate and special intervention by governments, international organizations, the private sector, philanthropic organizations, and civil society are needed.[80] It is estimated that by 2050, failing to tackle AMR may cost 10 million premature deaths per year and $100 trillion in cumulative economic damage.[81]
The dearth of effective treatments for neglected tropical diseases is also a key example of the failings of the existing drug development paradigm. Buruli ulcer, for example, is a painful infection that affects over 30 countries. Combined antibiotics can treat the disease, but more innovative research is needed to develop an oral therapy to help scale-up effective disease control in poor settings.[82] In this way, a profit-driven R&D model runs counter to the right of everyone to the highest attainable standard of health. According to the Office of the United Nations High Commissioner for Human Rights (OHCHR), drug companies bear a responsibility to invest in research and development for neglected diseases through in-house R&D or support for external research.
Currently, the fear of damaging a medicine’s market share often discourages pharmaceutical companies from disseminating important information about new medicines. As a result, there is little transparency of research data and methods of drug development. This practice poses not only a health risk for medicines users, but it is also counterintuitive to the knowledge sharing and creative process needed to develop new drugs. Furthermore, limited information sharing effectively restricts oversight of drug research and knowledge exchange that will ultimately delay drug innovation. As stated in OHCHR’s Human Rights Guidelines for Pharmaceutical Companies, “The right to the highest attainable standard of health not only requires that existing medicines are accessible, but also that much-needed new medicines are developed as soon as possible. [emphasis added]”[83] In contrast to current practice, knowledge sharing is key to protecting patients from potentially harmful treatments and successfully developing new medicines.
Ultimately, the current model of innovation delivers inaccessible medicines at prices that have become unaffordable for low-, middle-, and high-income countries alike. The field of cancer care is one example of the need for effective and affordable treatments across the globe, including in low- and middle-income countries where cancer rates are on the rise.[84] A vial of trastuzumab (Herceptin®), a medicine for breast cancer recently added to the WHO Essential Medicines List, reportedly costs 15 times the per capita monthly income in India (2014);[85] meanwhile, it runs up to 50,000 UK pounds to treat one patient for a year (2012).[86] Some companies justify these exorbitant prices by asserting they are warranted by heavy research and development costs. However, this argument fails to consider the many breakthrough essential medicines that were developed with government (tax-based) funding and/or in public-funded laboratories.[87] In these cases where the fruits of drug development are patented and privately licensed, the public effectively pays twice: first to subsidize medical research, and again, to access the new medicine.
Contrary to the notion of the universality of the right to health, the CEO of pharmaceutical firm Bayer criticized India’s compulsory license for the cancer drug sorafenib (Nexavar®): “We did not develop this medicine for Indians. We developed it for Western patients who can afford it.”[88] This business model becomes all the more egregious considering “5 percent of global resources for cancer are spent in the developing world, yet these countries account for almost 80 percent of disability-adjusted years of life lost to cancer globally.”[89] Addressing this paradox, Paul Farmer, co-founder of Partners in Health, has observed, “The market fails when it comes to research and development of drugs for the poor.”[90]
Several innovative solutions for medicines R&D were tabled to the United Nations Secretary-General’s High Level Panel on Access to Medicines in 2016. The panel was tasked with assessing proposals to resolve the policy incoherencies between IP law and trade rules on the one hand, and human rights law and public health needs on the other.[91] Among the submissions they received was a proposal for an “Essential Medicines Patent Pool” that can allow for more affordable generics to be produced for communicable and non-communicable diseases while also remunerating patent holders.[92] Another recommendation was to initiate a global treaty on biomedical R&D to allow governments to collectively pool funding, coordinate, and monitor research in a way that delinks the price of new medical products from research and development costs, thereby improving the affordability of health technologies.[93] A radically new approach, “Health Innovation as a Public Good,” aims to “generate cheaper medicines for all public health needs” by shifting leadership, priority setting, and research financing to the public sector, which would result in public goods and eliminate the need for profit.[94] These and other proposals were considered before the High Level Panel released its Final Report in September 2016.
The Final Report provided a combination of high-level and highly specific recommendations for reform. With respect to TRIPS, the High Level Panel (HLP) reiterated existing calls for greater use of the public health flexibilities available under TRIPS but went slightly further; it cautioned governments and the private sector to refrain from threats, tactics, or strategies designed to undermine the use of TRIPS flexibilities by developing nations and recommended that any instances of undue pressure be reported to the WTO Secretariat during the Trade Policy Review of Member States and be met with punitive measures.
With respect to research and development, the HLP recommended the negotiation of a binding R&D convention that would delink the costs of R&D from end product prices and redirect R&D to pressing public health needs, including neglected tropical diseases and antimicrobial resistance.
With respect to global health governance, accountability, and transparency, the HLP recommended that (a) Member States improve institutional coherence between trade, IP and public health at the national level; (b) an independent review body and an inter-agency task force be developed by the UN Secretary-General to assess progress on health technology innovation and access, and increase coherence between multilateral organizations, respectively; and (c) private biomedical companies report annually on actions taken to promote access to health technologies, and engage in transparent disclosure of the costs of R&D, marketing, and distribution, and any public funding received in the development of health technologies.
The many, varied recommendations of the High Level Panel illustrate the complex challenges produced by the interaction between intellectual property, international trade, international human rights, and public health. Importantly, they demonstrate that the incoherencies between these spheres of influence can only be resolved using robust accountability frameworks that hold all stakeholders responsible for the impact of their actions on access to affordable health technologies.[95]
2. Non-discrimination and equality
Access to medicines remains an illusory goal for traditionally marginalized groups. However, non-discrimination and equality – two of the most fundamental principles under human rights law – is central to the right to health.[96] Under the ICESCR, access to medicines should be realized without distinction on the grounds of race, color, sex, language, religion, political or other opinion, national or social origin, property, disability, birth or other status.[97] The International Convention on the Elimination of All Forms of Racial Discrimination also emphasizes that states must prohibit and eliminate racial discrimination in the enjoyment of public health and medical care.[98] Failure to comply with these standards amounts to a violation of international law.[99],[100]
However, non-discrimination and equality do not always imply equal treatment.[101] In some cases, states must assume positive obligations to prioritize underrepresented individuals and communities.[102] For example, certain populations face particular health challenges, including higher mortality rates or barriers to access, that must be reflected in national health policies.[103]
People living with HIV and AIDS[104]
Navi Pillay, former UN High Commissioner for Human Rights, has stated, “The face of HIV has always been the face of our failure to protect human rights.” HIV/AIDS is a global epidemic. More than 30 million people have died of AIDS, and there are approximately 36.9 million people living with HIV today.[105],[106] Each year, some 2.5 million people become infected with HIV, and around 1.7 million people die of AIDS-related causes, mostly in low- and middle-income countries.[107]
HIV/AIDS disproportionately affects people living in developing countries and persons living in poverty. This distribution is deeply rooted in social, economic, and gender inequalities. Sub-Saharan Africa remains the worst-affected region, with 69% of all persons living with HIV/AIDS.[108] The Caribbean region has the highest HIV prevalence outside of sub-Saharan Africa, and the number of new HIV infections is increasing in Eastern Europe, Central Asia, North Africa, the Middle East, and parts of Asia and the Pacific.[109]
HIV is treated with antiretroviral (ARV) therapy, which is a combination formula of at least three antiretroviral drugs that maximally suppress the HIV virus and halt the progression of the HIV disease.[110] ARV therapy is effective both as life-saving treatment and as protection against HIV/ AIDS. However, coverage for people living with HIV/AIDS remains unequal, and in 2011, just 54% of people indicated for ARV in low- and middle-income countries received the treatment. Globally, just 28% of children in need of treatment received ARV.[111]
Although there is not yet universal access in many countries, treatment has been successful in extending life expectancy, decreasing HIV transmission, and promoting community activism and empowerment around HIV/AIDS and the protection of human rights. According to the Global Commission on HIV and the Law, “Legal strategies, together with global advocacy and generic [drugs], resulted in a 22-fold increase in ART access between 2001 and 2010.” These legal strategies included framing lack of access to ARV as a breach of human rights. Civil society action, such as that of the Treatment Action Campaign in South Africa, held national governments accountable to their legal obligations in international law and their domestic constitutions These strategies can be replicated to access treatment for other epidemics.
A number of mechanisms are also available to help make HIV medicines more affordable. These include robust generic competition, local production, voluntary licensing by innovator to generic companies, and the use of flexibilities in the international trade and intellectual property rules (through the TRIPS Agreement and other WTO mechanisms) to achieve wider access to affordable generic medicines. One such flexibility is compulsory licensing, which is permitted by TRIPS Article 31. Under a compulsory license, the issuing government sets the terms upon which a third party can exploit a patented product without the patent holder’s consent. The patent holder receives adequate remuneration and retains exclusive rights over the patented good, except with respect to the compulsory licensee. Compulsory licenses have been an integral component of patent law for centuries, and have been used extensively by countries around the world.[112] Canada’s highly permissive compulsory licensing regime facilitated significant price reductions in pharmaceutical drugs,[113] and helped to establish a robust generic manufacturing industry before it was dismantled by NAFTA in the early 1990s.[114] Since the start of the 21st century, a number of developing countries have either issued or threatened to issue compulsory licences on pharmaceutical products to expand access to affordable medicines, including Thailand, Brazil, Rwanda, Indonesia, Malaysia, Zambia, Zimbabwe, and Mozambique.[115]
There are numerous advantages associated with compulsory licensing for pharmaceutical drugs, including, inter alia, the ability to achieve significant price reductions long before the expiry of the patent term; the reduction in dependence on a sole supplier; and the ability to respond swiftly to public health emergencies. In 2015, South Africa experienced severe shortages of Lopinavir/ritonavir (LPV/r), a combination antiretroviral medicine used in first-line ARV regimens for paediatric patients, and second-line regimens for adults and adolescents who have developed resistance to first-line treatments. The drug is marketed as “Aluvia” by patent holder AbbVie, which is the sole supplier in South Africa.[116] The shortages resulted from AbbVie’s inability to deliver adequate supplies, and resulted in significant treatment disruptions for HIV patients. Treatment disruptions place HIV patients at risk of developing drug resistance and immunological failure. Patients who develop resistance to second-line treatment must be switched to third-line treatment, which is six times more expensive.[117] Although generic versions of Aluvia were already prequalified by the World Health Organisation, they could not be produced in, or imported into, South Africa until the expiry of AbbVie’s patent in 2028.[118] The shortages triggered significant public outcry, and civil society organizations called for the South African government to issue a compulsory license on Aluvia.[119] No such license was issued. Cases like these have prompted widespread calls for governments to “adopt and implement legislation that facilitates the issuance of compulsory licenses. Such legislation must be designed to effectuate quick, fair, predictable, and implementable compulsory licenses for legitimate public health needs, and particularly with regards to essential medicines”.[120]
As countries continue to confront new challenges in the fight against HIV/AIDS, compulsory licensing will continue to be a critical tool for sustainable access to affordable antiretroviral treatment. Namibia, for example, has one of the highest antiretroviral treatment (ART) coverage rates in sub-Saharan Africa (at 90%) but the country is increasingly struggling to combat HIV drug resistance (HIVDR) which requires second-line ART regimens with long-term toxicity and higher annual costs. There are widespread concerns about the sustainability of Namibia’s ART program given its heavy reliance on donor funds. Accordingly, compulsory licensing is critically needed to maintain drug-supply continuity and facilitate the development of local pharmaceutical manufacturing capacity.
Children
Every year, over eight million children under five years of age die, many from illnesses such as diarrhea, malaria, HIV/AIDS, tuberculosis and pneumonia.[121] Children and young people are also among the worst affected by the HIV epidemic, in large part due to mother-to-child transmission and slow progress in the prevention, diagnosis, and treatment of HIV in children specifically. Due to interrelated biological and social reasons—contact with infected persons, being less than five years of age, and severe malnourishment—children are also especially vulnerable to TB. Each year, there are approximately 500,000 new TB cases and up to 70,000 TB deaths among children.[122]
As a particularly vulnerable, and often silent, subset of the population, children face unique challenges that prohibit them from enjoying the right to health, including access to child-friendly drugs. For instance, although effective treatments have been developed for many of the major diseases that affect children, often pediatric versions of these treatments do not exist. Children require dosages that are reflective of their age, physical condition, and body weight.[123] Though it is common for healthcare providers to split adult dosages into halves or quarters for children’s use, these makeshift tablets risk inaccurate dosing, thereby reducing the efficacy and/or safety of the treatment.[124]
Adult sized medicines are also often unpalatable and difficult to digest for children. Oral solutions and syrups are more tolerable, and yet medications in these forms are usually unavailable, too expensive, or unsuitable for use in low-income settings. For diseases requiring several treatments per day—HIV/AIDS is one example—a fixed dosage combination approach is ideal. However, these combination pills are much more expensive than their adult counterparts.[125] To address some of these gaps, pediatric ARV drug development projects have been initiated. Generic companies also have been able to develop formulations for children.
Prior to 2006, few strides had been made in the research and development of child-friendly medicines. The difficulty of administering clinical trials on children made advances even more difficult.[126] However, in 2006, civil society organizations and governments began to partner in a quest to develop safer and better quality medicines specifically tailored to a child’s unique needs.[127] Improvements have been slow but steady. For instance, in 2007 WHO launched a campaign to remove some of these barriers, publishing the WHO Model List for Essential Medicines for Children and launching a campaign to promote the use of child-friendly tablets.
Women
Women are particularly vulnerable to violations of their rights in seeking access to medicines, especially for sexual and reproductive health care services. For example, women in many developing countries face a shortage of prophylactic uterotonics, a drug that helps to prevent and treat Postpartum Haemorrhage (PPH). PPH, defined as a blood loss of 500 ml or more within 24 hours after birth, is the leading cause of maternal mortality globally.[128] Without access to prophylactic uterotonics during the third stage of labor, scores of women in low-income countries suffer from long-term disability, contract severe maternal conditions associated with substantial blood loss, and/or die preventable deaths. It is therefore unsurprising that the provision of essential medicines for sexual and reproductive health is a “core” duty of the state in the CESCR’s General Comment 22 on the right to sexual and reproductive health.[129]
Women and girls who have been trafficked for prostitution are especially vulnerable to HIV/AIDS and sexually transmitted infections and require access to medicines on a non-discriminatory basis. In its General Recommendation on “Women and Health,” the Committee to Eliminate Discrimination Against Women (“CEDAW”) noted:
“The issues of HIV/AIDS and other sexually transmitted diseases are central to the rights of women and adolescent girls to sexual health. Adolescent girls and women in many countries lack adequate access to information and services necessary to ensure sexual health. . . . States parties should ensure, without prejudice or discrimination, the right to sexual health information, education and services for all women and girls.”[130]
In some cases, discrimination against women in their pursuit of medicines can be blatant. For instance, as the chapter on patient care has noted, Human Rights Watch documented abuses committed by health personnel who had deliberately refused to give pain-relieving medication to women while in labor.[131]
The Special Rapporteur on the right to health states, “Stigma and discrimination against women from marginalized communities, including indigenous women, women with disabilities and women living with HIV/AIDS, have made women from these communities particularly vulnerable to such abuses.”[132] Female patients from marginalized populations have the right to seek health care, and goods that promote health (i.e. medicines), in a manner that is non-discriminatory and respects their dignity.
More recently, the Zika epidemic highlighted the systemic discrimination suffered by women in exercising their right to health. Laws and policies in Zika-affected countries which significantly curtail female reproductive rights thereby violate the right to health and the right to life enjoyed by both mother and child, given the proven link between Zika infection and microcephaly. The UN High Commissioner for Human Rights, Zeid Ra’ad Al Hussein, has repeatedly called for the repeal of laws that restrict access to sexual and reproductive health services to ensure that women have the information, support and services they require to exercise their rights to determine whether and when they become pregnant.[133]
Prisoners/ detained persons
The right to health in prison lies at the nexus of positive and negative rights in the sense that, having deprived prisoners of their liberty and their ability to provide for their own health, states bear a positive obligation to protect their right to life and their right to health. Prisoners and detained persons in most countries do not relinquish their rights when they enter the jail system. However, since they are in many ways dependent upon the prison system, this population often faces violations of their rights, including the right to access medicines. [134]
Prison environments render their occupants more susceptible to certain diseases.
For example, although many prisoners living with HIV contracted their infections before imprisonment, the risk of infection while in prison is high due to high-risk sexual and other behaviors, like sharing needles. High-risk sexual behaviors, including unprotected sex and sexual violence, rape, and coercion, are common in prison and increase prisoners’ vulnerability to HIV. Unsafe drug injection, blood exchange, and the use of non-sterile needles/cutting instruments for tattooing are also common and increase HIV vulnerability. Poor prison conditions, including overcrowding, malnutrition, poor security, and lack of health facilities and staff, contribute to the spread of HIV and violate prisoners’ human rights.
Some prisons create separate or alternative sections for HIV-positive prisoners, segregating them from the rest of the prison population. In parts of Russia, prisoners are tested for HIV and those who test positive are imprisoned together, but separated from the general prison population. Two states in the United States, Alabama and South Carolina, continue to segregate prisoners living with HIV. The American Civil Liberties Union and the AIDS Project recently filed a lawsuit calling the practice discriminatory.[135] Their reports highlight additional human rights violations that are consequences of discriminatory segregation.[136]
In addition, prisoners are by definition not free individuals who can go to the pharmacy, and they are dependent on others to physically provide medicines. Prisoners also often have little or no means to finance medicines, so they must be funded by the prison system. Both of these obstacles routinely obstruct prisoners from realizing their right to access medicines. For instance, due to high costs, it has been documented that prison systems have withheld newer medications, including drugs for Hepatitis C, from patients in need. Several such cases have been documented in the United States, including in Rhode Island, Massachusetts, and Minnesota.[137]
The prison population includes vulnerable groups with special needs, including prisoners with mental health care needs, elderly prisoners, and prisoners with terminal illness. These vulnerable populations may require special attention to ensure that their rights to health and life with dignity are realized.
Older persons
Older persons are a vulnerable group and more susceptible to issues related to non-communicable diseases (NCDs) and pain management control. NCDs, such as cancer, heart disease, and diabetes, affect many people—but especially older people. NCDs prevention and treatment can also demand a chronic (and expensive) course of medicine that may not be available or affordable for this population.[138] Because government-funded medicines are often the only source of treatment for this population, many of these patients must pay out-of-pocket to access medicines for their chronic conditions. These sometimes catastrophic expenses can force older patients to have to choose between medicines they need and their financial stability.[139] The problem becomes even more acute when one considers the new, expensive medicines with proven therapeutic value to treat cancer. This raises an ethical and economic dilemma for industrialised and developing countries alike of how to afford these high-cost, therapeutically-innovative medicines.
In developing countries, the affordability and accessibility of chronic and/or expensive pharmaceuticals is especially limited, and in many cases, unaffordable medicines leave older people with pain control as the only viable treatment. However, opioids needed to control pain are subject to additional regulation that restricts their much-needed use. While the international drug control framework, which includes the Single Convention on Narcotic Drugs, the Convention on Psychotropic Substances, and the United Nations Convention on Illicit Traffic in Narcotic and Psychotropic Drugs, has been crafted to combat illicit drug markets, it is incoherent with obligations that derive from human rights law. The restrictive interpretation of the control mechanisms included in the international drug control treaties directly hinder states access to controlled substances for medical purposes.[140]
The United Nations Committee on Economic, Social and Cultural Rights states that, with regard to the realization of the right to health of older persons, “attention and care for chronically and terminally ill persons [is important], sparing them avoidable pain and enabling them to die with dignity.” Therefore, an important component of palliative care is access to essential drugs that alleviate pain.
In 2007, the International Association for Hospice and Palliative Care (IAHPC), in collaboration with 26 palliative care organizations, developed a list of essential medicines for palliative care.[141] Of the 34 medications listed, just 14 were included in the WHO Model List (most recently updated in 2011), and morphine was the only strong opioid analgesic included. Oral morphine is particularly essential for palliative care because it provides an inexpensive option for pain management. However, especially in low- and middle- income countries, only opioid formulations that are more expensive or more difficult to use, such as injectable morphine, are available. The high cost of these opioids hinders access to treatment. Meanwhile, the low profit margin from oral morphine is exacerbated by additional costs of unnecessarily burdensome regulatory requirements, which may further deter the pharmaceutical industry from supplying it.[142]
Persons living with neglected diseases[143]
Neglected diseases are diseases for which there is a lack of sufficient medical innovation, resulting in inadequate, ineffective, or non-existent means to prevent, diagnose and treat them. The lack of sufficient medical innovation is often caused by a lack of market incentives to invest in products that will predominantly be directed towards populations with little or no purchasing power.[144] Examples include: leishmaniasis, schistosomiasis, onchocerciasis, lymphatic filariasis, Chagas disease, malaria, leprosy, African trypanosomiasis, tuberculosis and dengue.[145]
Neglected diseases are demonstrative of entrenched global inequities that perpetuate disparities in the enjoyment of the right to health between the rich and the poor. For example, although the situation has improved, drug development efforts have largely focused on diseases with a higher return than those that afflict predominantly poor populations.
Through international cooperation and research and development,[146] states bear the responsibility to improve the underlying determinants of health that predispose certain populations to these diseases.[147] More immediately, governments and civil society must pressure pharmaceutical companies to produce medicines that address neglected diseases. For example, the African Union Commission has suggested these activities should include “giving large pharmaceutical firms incentives to investigate the diseases that affect Africa, instead of focusing on the diseases of rich countries.”[148]
Neglected diseases do not only suffer from lack of R&D funding. The patenting of basic scientific research tools, such as gene fragments, does not allow developing world scientists to benefit from accumulated research. Publishers often price their copyright journals beyond the means of the Global South, wherein scientists are denied the right to information and developing countries subsequently do not benefit from the right to scientific progress and research.
What are rights-based interventions and practices in the area of access to medicines?
Operationalizing a human rights framework is an essential approach toward advancing access to medicines. This multi-pronged approach should involve participation and coordination between governments, philanthropic organizations, international entities, civil society groups, and the private sector.
To start, programmatic reforms to increase access must be incorporated in national policies and programs, with special consideration for populations that routinely face access barriers, such as incarcerated persons, women, children, and those affected by diseases that can only be treated with high priced medicines. Equally, the prioritization of access to essential medicines must be reflected in new rights-based laws and licensing the products of medical research. In addition, states, especially in the Global South, should fully utilize the public health flexibilities available under TRIPS to address their country’s specific domestic health needs. A number of other mechanisms are available to help make medicines more affordable. Some of these methods include promoting generic competition, local production, and voluntary licensing by innovator to generic companies. Pharmaceutical companies should respect the right of states to use TRIPS flexibilities and refrain from pursuing stronger intellectual property protection than that is required by TRIPS. Initiatives to increase access to medicines must also bear in mind the principle of transparency, so that accountability frameworks can hold all stakeholders to account and better address the misalignment between the right to health, trade, intellectual property, and public health objectives.[149]
A human rights approach must also be supported by robust international assistance and cooperation, especially where public health objectives cannot be fulfilled immediately by the state.[150] As part of the tripartite classification of obligations for all human rights, experts increasingly contend that the duty to fulfill rights suggests that developed countries have positive duties beyond borders.[151] According to the CESCR, developed countries have a responsibility to contribute to contribute to countries in need, to “the maximum of [their] capacities,” in situations of emergency.[152] The courts can also play an important role in enforcing the right to health. In fact, right-to-health litigation to advance access to medicines exemplifies, in very practical terms, how human rights can be used to force governments to act.
The strategies outlined below all strive to increase access to medicines for all. Some of these strategies are ongoing, and should continue or be scaled up.
Official and non-governmental initiatives and international assistance
The right to health obliges states to advance access to medicines through international assistance and cooperation.[153] To help meet these commitments, the Global Fund to Fight AIDS, Tuberculosis and Malaria, an independent, multilateral financing entity, was conceived in 2002. The Global Fund directs resources to countries to support their response to HIV/AIDS, tuberculosis, and malaria and is the largest multilateral funder program that provides access to treatments those diseases.[154] UNITAID, an international drug purchasing financing facility, has been another pioneering initiative. Through multilateral coordination and strategic market interventions, UNITAID creates and improves upon incentives for the pharmaceutical sector to better meet the world’s health needs.[155] Finally, the United States President’s Emergency Plan for AIDS Relief, otherwise known as PEPFAR, is another health financing mechanism, which has been instrumental in curtailing the HIV/AIDS epidemic by supporting ART treatment for nearly 9.5 million people worldwide as of September 2015.[156]
This concept, which describes a financing model characterized by the uncoupling of R&D costs and consumer prices for health technologies, is known as “delinkage.”[157] A joint WTO, WIPO, WHO study described “delinkage” in the following terms: “One important concept that evolved from this discussion is the concept of delinking price of the final product from the costs of R&D. This concept is based on the fact that patents allow developers to recoup the costs and make profits by charging a price in excess of the costs of production. This way of financing R&D is viewed as constituting a barrier to access to medicines in countries where populations pay out of their own pockets for medicines and thus cannot afford to pay high prices. The principle of delinking is based on the premise that costs and risks associated with R&D should be rewarded, and incentives for R&D provided, other than through the price of the product.”[158]
As the world moves to curtail the spread of diseases beyond HIV/AIDS, primarily for diseases that are not incentivized by a robust market, innovation models should actively seek to “delink” R&D costs from the end price of products and share the burden of these costs on an international scale. As the 2016 UNHLP has stated, the current “patchwork” of public, private, and philanthropic funding is not sufficient enough to sustain long-term public health financing.[159] New proposals have included using the WHO as a galvanizing force to “initiate international talks about priority setting and burden sharing of the cost of essential health R7D and set new rules to allow for financing of innovation while equitable access to those innovations is assure. This would initiate international implementation of delinkage.”[160] A subsequent adoption of a new medical R&D framework could also include the following elements: “R&D priorities driven by health needs; Binding obligations of governments to invest in health R&D; Equitable distribution of contributions across countries; Measures to improve the regulatory environment and collaboration; Measure to ensure affordability of the end product; Access-maximising licensing practices to deal with IP issues; and Innovative approaches to incentivising R&D based on linkage principles.”[161]
Governance and flexibilities allowed under TRIPS
World Trade Organization (WTO) Members must make full use of TRIPS flexibilities to promote access to medicines. In accordance with Article 8 of the agreement, states may “adopt measures necessary to protect public health” as they “[formulate] or [amend] their laws and regulations.” States should also take advantage of “the policy space available in Article 27… by adopting and applying rigorous definitions of invention and patentability that are in the best interests of the public health of the country and its inhabitants.”
Flexibilities must be explicitly incorporated into national policies and legislation. In particular, laws should be amended to promote compulsory licensing, permit parallel importation, promote pre-grant opposition, strengthen antitrust remedies for abuse of monopoly power, and strengthen patentability criteria to ensure that patents are only awarded “when genuine innovation has occurred.”[162]
Pharmaceutical policy reform
As Ministers and senior public officials have suggested,[163] pharmaceutical companies can and should exercise good corporate governance. They can do so by adopting the OHCHR’s Human Rights Guidelines for Pharmaceutical Companies, including:
-
The company should adopt a human rights policy statement which expressly recognises the importance of human rights generally, and the right to the highest attainable standard of health in particular, in relation to the strategies, policies, programmes, projects and activities of the company;
-
The company should integrate human rights, including the right to the highest attainable standard of health, into the strategies, policies, programmes, projects and activities of the company;
-
The company should always comply with the national law of the State where it operates, as well as any relevant legislation of the State where it is domiciled;
-
The company should refrain from any conduct that will or may encourage a State to act in a way that is inconsistent with its obligations arising from national and international human rights law, including the right to the highest attainable standard of health.”[164]
Pharmaceutical companies are responsible for investing in research and development to benefit all patients. In the realm of competition and pricing, companies can engage in fair market practices.[165] For instance, in 2014, Gilead issued a voluntary license for sofosbuvir to generic producers, a treatment for Hepatitis C, which allows production and supply of generic SOF to 101 countries for this disease. Although this is a positive step for 101 nations, Gilead’s license still excludes countries where 73 million people with the Hepatitis C virus live. This move effectively leaves out 46% of HCV patients globally from an agreement that can deliver more affordable generic treatment and allows supply to other countries in the event that, for instance, a compulsory license is issued.[166]
Health systems strengthening
Access to medicines fundamentally depends upon well-functioning health systems. According to guidelines set out by the OHCHR, systems must be “integrated, responsive, and accessible.”[167] Governments should scale up their investment in these systems, as well as scale up transparency and participatory priority-setting for drug spending.
Governments should also erect strong regulatory systems to ensure medicines are safe, effective, and of assured quality. A well formulated and comprehensive National Medicines Policy (NMP), as laid out by WHO, can guide governments to set priorities for the national pharmaceutical sector that satisfy their human rights obligations.[168] A national essential medicines list outlines the most clinically- and cost-effective medicines for priority diseases. When used within a health system, a national essential medicines list can help limited drug budgets achieve the greatest public health impact. In line with the principle of progressive realization, governments should continuously increase the public funding available for essential pharmaceuticals, especially considering many of the most marginalized populations either pay out of pocket or make do without these medicines.
Claim health rights before domestic or regional courts
The courts can also play a role in promoting health rights, including addressing the affordability and accessibility of medicines.[169] This intervention in particular shows, in very practical terms, how human rights can be used as a tool to force the government to act.
The claims of individuals or groups have been particularly efficacious when access to medicines is linked to a country’s constitutional right to health or human rights treaties (including the right to health) ratified by the government. For example, a study identified that state recognition of the right to health in international or domestic law created a supportive environment for cases in which access to essential medicines was claimed as a derivative of the right to health and thereby reinforcing the enforceability through domestic courts.[170]
Two case studies at the end of this chapter, based in Kenya and Georgia respectively, highlight recent trends in litigation concerning access to medicines. Both examples indicate that support from non-governmental organizations can help shepherd the likelihood of success. Secondly, it might be inferred that judges are increasingly ruling in favor of the protection of patient’s rights over the enforcement of patents.[171]
Though an uptake in the amount of cases litigating the right to medicines in national courts has been documented, the extent that this movement has on the right to health as a whole has yet to be determined.[172],[173]
2. Which are the most relevant international and regional human rights standards related to access to medicines?
How to read the tables
Tables A and B provide an overview of relevant international and regional human rights instruments. They provide a quick reference to the rights instruments and refer you to the relevant articles of each listed human right or fundamental freedom that will be addressed in this chapter.
From Table 1 on, each table is dedicated to examining a human right or fundamental freedom in detail as it applies to patient care. The tables are organized as follows:
| Human right or fundamental freedom | |
| Examples of Human Rights Violations | |
|
Human rights standards
|
UN treaty body interpretation This section provides general comments issued by UN treaty bodies as well as recommendations issued to States parties to the human right treaty. These provide guidance on how the treaty bodies expect countries to implement the human rights standards listed on the left. |
| Human rights standards |
Case law This section lists case law from regional human rights courts as well as from the country level. Case law creates legal precedent that is binding upon the states under that court’s jurisdiction. Therefore it is important to know how the courts have interpreted the human rights standards as applied to a specific issue area. |
|
Other interpretations: This section references other relevant interpretations of the issue. It includes interpretations by: – UN Special Rapporteurs – UN working groups – International and regional organizations – International and regional declarations |
|
The tables provide examples of human rights violations as well as legal standards and precedents that can be used to redress those violations. These tools can assist in framing common health or legal issues as human rights issues, and in approaching them with new intervention strategies. In determining whether any human rights standards or interpretations can be applied to your current work, consider what violations occur in country and whether any policies or current practices in your country contradict human rights standards or interpretations.
Human rights law is an evolving field, and existing legal standards and precedents do not directly address many human rights violations. Through ongoing documentation and advocacy, advocates can build a stronger body of jurisprudence on human rights in patient care.
In the tables, we use the following abbreviations to refer to the nine treaties and their corresponding enforcement mechanisms:
Also cited are the former Commission on Human Rights (CHR) and various UN Special Rapporteurs (SR) and Working Groups (WG).
Table A: International Human Rights Instruments and Protected Rights and Fundamental Freedoms
|
|
UDHR | ICCPR | ICESCR | CEDAW | ICERD | CRC | ||||||||
| Liberty and Security of Person | Art. 3 | Art. 9(1) | Art. 5(b) | |||||||||||
| Non-Discrimination and Equality | Art. 1, Art. 2 | Art. 2(1), Art. 3 | Art. 2(2), Art. 3 | Art. 2, All | Art. 2, Art. 5, All | Art. 2 | ||||||||
| Life | Art. 3 | Art. 6(1) | Art. 6(1) | |||||||||||
| Health | Art. 25 | Art. 12 | Art. 12 | Art. 5(e)(iv) | Art. 24 | |||||||||
| Abuse, Torture, and Ill-Treatment* | Art. 5 | Art. 7 | Art. 37(a) | |||||||||||
| Expression and Information | Art. 19 | Art. 19(2) |
Art. 13, Art. 17 |
|||||||||||
| Enjoy Benefits of Scientific Progress | Art. 27 | Art. 15 | ||||||||||||
| Women | Art. 16, Art. 25(2) | Art. 3, Art. 23 | Art. 3, Art. 10(1), Art. 10(2) | All | ||||||||||
| Children | Art 25(2) | Art. 24 | Art. 10(3), Art. 12(2)(a) | Art. 5(b) | All | |||||||||
*See also Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment, Article 2.
Table 1: Access to Medicines and the Right to Non-Discrimination and Equality
| Examples of Human Rights Violations |
|
· Zimbabwean prisoners in Botswana are denied access to antiretroviral (ARV) therapy to control their HIV infection and reduce opportunistic maladies while HIV positive Botswanan prisoners in the same institution are supplied with treatment. · The Venezuelan Ministry of Defence denied HIV positive soldiers access to ARVs. But when the soldiers brought the case before court, the court voluntarily extended its decision to provide ARVs all infected members of the army. Only through subsequent litigation was access to ARVs and laboratory tests extended to all people with HIV, including civilians and those not eligible under existing health programmes. |
| Human Rights Standards | Treaty Body Interpretation |
|
ICERD 5(e)(iv) States Parties undertake to prohibit and to eliminate racial discrimination in all its forms and to guarantee the right of everyone, without distinction as to race, colour, or national or ethnic origin, to equality before the law, notably in the enjoyment of the following rights: (e) Economic, social and cultural rights, in particular: (iv) The right to public health, medical care, social security and social services. |
|
|
ICESCR 2(2) The States Parties to the present Covenant undertake to guarantee that the rights enunciated in the present Covenants will be exercised without discrimination of any kind as to race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status. ICESCR 12(1) The States Parties to the present Covenant recognize the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. |
CESCR General Comment 20: In explaining “other status” under ICESCR 2(2), CESCR explains “Health status refers to a person’s physical or mental health. States parties should ensure that a person’s actual or perceived health status is not a barrier to realizing the rights under the Covenant. The protection of public health is often cited by States as a basis for restricting human rights in the context of a person’s health status. However, many such restrictions are discriminatory, for example, when HIV status is used as the basis for differential treatment with regard to access to education, employment, health care, travel, social security, housing and asylum. States parties should also adopt measures to address widespread stigmatisation of persons on the basis of their health status, such as mental illness, diseases such as leprosy and women who have suffered obstetric fistula, which often undermines the ability of individuals to enjoy fully their Covenant rights. Denial of access to health insurance on the basis of health status will amount to discrimination if no reasonable or objective criteria can justify such differentiation.” E/C.12/GC/20 (June 10, 2009). CESCR General Comment 14: “With respect to the right to health, equality of access to health care and health services has to be emphasized. States have a special obligation to provide those who do not have sufficient means with the necessary health insurance and health-care facilities, and to prevent any discrimination on internationally prohibited grounds in the provision of health care and health services, especially with respect to the core obligations of the right to health.” CESCR General Comment No. 14 (14): Explaining that “health facilities, goods and services must be accessible to all [without discrimination], especially to the most vulnerable and marginalized sections of the population . . . .” The Committee stated that this included the health care access needs of “ethnic minorities and indigenous populations, women, children, adolescents, older persons, persons with disabilities and persons with HIV/AIDS.” |
| CEDAW 12(1) States Parties shall take all appropriate measures to eliminate discrimination against women in the field of health care in order to ensure, on a basis of equality of men and women, access to health care services, including those related to family planning. | CEDAW General Recommendation No. 24 (12) (Women and Health): Affirming that “access to health care, including reproductive health, is a basic right under the Convention on the Elimination of All Forms of Discrimination against Women” and that States must “eliminate discrimination against women in their access to health-care services throughout the life cycle, particularly in the areas of family planning, pregnancy and confinement and during the post-natal period.” |
| Human Rights Standards | Case Law |
| Constitution of Botswana 15: (1) Subject to the provisions of subsections (4), (5) and (7) of this section, no law shall make any provision that is discriminatory either of itself or in its effect. (2) Subject to the provisions of subsections (6), (7) and (8) of this section, no person shall be treated in a discriminatory manner by any person acting by virtue of any written law or in the performance of the functions of any public office or any public authority. (3) In this section, the expression “discriminatory” means affording different treatment to different persons, attributable wholly or mainly to their respective descriptions by race, tribe, place of origin, political opinions, colour or creed whereby persons of one such description are subjected to disabilities or restrictions to which persons of another such description are not made subject or are accorded privileges or advantages which are not accorded to persons of another such description. |
High Court of Botswana: Finding that the denial of Highly Active Antiretroviral Therapy to non-citizen inmates due to a Presidential Directive stating that the State must provide “free treatment to non citizen prisoners suffering from ailments other than AIDS” was unconstitutional as it violated the right to life (Section 4), the right to freedom from torture (Section 7), and the right to non-discrimination (Section 15). Tapela & Ors. v. Attorney General and Ors. (MAHGB-000057-14), BWHC 1 (2014). |
| Constitution of Argentina (No specified articles). | Supreme Court of Argentina: Court rules to protect the right of life, right of health, and right to avoid discrimination of HIV-positive man after being denied the independent continuation of insurance coverage after his job termination and after the company learns of his condition. V., W. J. v. Obra Social de empleados de Comercio y Actividades Civiles. V. 1389. XXXVIII (2004). |
| Constitution of the Oriental Republic of Uruguay 8: All persons are equal before the law, no other distinctions being recognized among them save those of talent and virtue. | Third Civil Appellate Court of Uruguay: Finding that the Ministry of Public Health’s failure to provide drug Cetuximab to colon cancer patient because it was not listed in the Therapeutic Drug Registry violated the principle of equality because it had been given to others in similar circumstances. Sentencia No. 03/2011. |
| Other Interpretations |
|
Convention (No. 169) Concerning Indigenous and Tribal Peoples in Independent Countries, ILO, art. 7(2) (June 27, 1989): States parties should “ensure that adequate health services are made available to the [indigenous and tribal] peoples concerned.” Declaration of Commitment of HIV/AIDS: By 2003, enact, strengthen or enforce, as appropriate, legislation, regulations and other measures to eliminate all forms of discrimination against and to ensure the full enjoyment of all human rights and fundamental freedoms by people living with HIV/AIDS and members of vulnerable groups, in particular to ensure their access to…prevention, support and treatment. United Nations Declaration on the Rights of Indigenous Peoples, Art. 24: (1) Indigenous peoples have the right to their traditional medicines and to maintain their health practices, including the conservation of their vital medicinal plants, animals and minerals. Indigenous individuals also have the right to access, without any discrimination, to all social and health services … (II) Indigenous individuals have an equal right to the enjoyment of the highest attainable standard of physical and mental health. States shall take the necessary steps with a view to achieving progressively the full realization of this right. |
Table 2: Access to Medicines and the Right to Life
| Examples of Human Rights Violations |
| · In government health facilities pregnant mothers can receive healthcare and medicines to deliver their babies. However, systematic shortages of critical medicines needed to control bleeding during and after childbirth can contribute to the needless death of new mothers. |
| Human Rights Standards | Treaty Body Interpretation |
|
ICESCR 12(1): “The States’ Parties to the present Covenant recognize the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.” “The steps to be taken by the States Parties to the present Covenant to achieve the full realization of this right shall include those necessary for . . . The prevention, treatment and control of epidemic, endemic, occupational and other diseases.”
|
CESCR General Comment 14: “With respect to the right to health, equality of access to health care and health services has to be emphasized. States have a special obligation to provide those who do not have sufficient means with the necessary health insurance and health-care facilities, and to prevent any discrimination on internationally prohibited grounds in the provision of health care and health services, especially with respect to the core obligations of the right to health.” |
| ICCPR 6(1): Every human being has the inherent right to life. This right shall be protected by law. No one shall be arbitrarily deprived of his life. | HRC General Comment No. 6 (1 and 5): Explaining that the right to life “should not be interpreted narrowly” or “in a restrictive manner,” and its protection “requires that States adopt positive measures . . . to increase life expectancy.” |
|
CRC 6(2): “States Parties recognize that every child has the inherent right to life” and “States Parties shall ensure to the maximum extent possible the survival and development of the child.”
|
CRC: Expressing to Cote d’Ivoire that “[w]hile noting the existence of the National Programme for the Control of AIDS, Sexually Transmitted Infections and Tuberculosis, the establishment of a special Ministry on HIV/AIDS, and the setting up of a committee on HIV/AIDS orphans, the Committee remains extremely concerned at the alarmingly high incidence and increasing prevalence of HIV/AIDS amongst adults and children and the resulting large number of children orphaned by HIV/AIDS.” CRC/C/15/Add.155 (2001) |
| Human Rights Standards | Case Law |
|
ECHR 2(1): Everyone’s right to life shall be protected by law. No one shall be deprived of his life intentionally save in the execution of a sentence of a court following his conviction of a crime for which this penalty is provided by law.
|
ECtHR: Holding that “this provision for the right to life requires states not only to prevent intentional killing but also to take steps against unintentional loss.” Tavares v. France, 16593/90 (September 12, 1991) (unreported), cited in Rebecca J. Cook & Bernard M. Dickens, Human Rights Dynamics of Abortion Law Reform, 25 HUM. RTS. Q. 1, 28 (2003). [AY]
|
| ACHPR 4(1). Every person has the right to have his life respected. This right shall be protected by law and, in general, from the moment of conception. No one shall be arbitrarily deprived of his life. | IACHR: The Court found the Nigerian government responsible for violating and failing to protect “such provisions as the right to life (Art. 4), the right to health (Art. 16) and the right to economic, social and cultural development (Art. 22). By its violation of these rights, the Nigerian government trampled upon not only the explicitly protected rights but also upon the right to food implicitly guaranteed.” Social and Economic Rights Action Center v. Nigeria, 155/96 (October 13-27, 2001), para. 67. |
| ACHR 4. “Every person has the right to have his life respected. . . . No one shall be arbitrarily deprived of his life.” | IACHR: “The right to life must be examined in its relationship to the commitment of the State, established in article 1(1), to respect and guarantee the full exercise of every right recognized in the [American] Convention.” Mendes v. Brazil (April 13, 1999), para.101. |
| Constitution of Bolivia (of 1967) 7: Every person has the following fundamental rights, in accordance with the laws which regulate their exercise: (a) to life, to health and social security. | Constitutional Tribunal: Finding a violation of the right to life (and health and social security) in the cessation by COSSMIL (the Military Social Security Corporation) to provide HIV patient with necessary medications that he was not able to afford on his own. The court extended a previous judgment covering the continued provision of medicines for those suffering chronic illnesses to those suffering from HIV/AIDS. Ana María Campero de Romero, Defensora del Pueblo v. Máximo García Bonilla, et al., General Manager of Health. Constitutional Judgment 26/2003-R. |
| Constitution of Colombia 49: Public health and environmental protection are public services for which the state is responsible. All individuals are guaranteed access to services that promote, protect, and rehabilitate public health. | The Colombian Constitutional Court established that “the right to health was enforceable when it was inextricably related to enabling a life of dignity – and not merely preventing imminent death” and on this doctrine has ordered antiretroviral and cancer medications, financing treatment abroad for acute leukemia, treatment of severe depression, post-mastectomy breast implants, administration of growth hormones, and care for severe vision problems. |
Table 3: Access to medicines and the right to the highest attainable standard of health
| Examples of Human Rights Violations |
|
· Venezuelans living with HIV lack the financial means to purchase antiretroviral medicines and the Ministry of Health & Social Assistance failed to provide this medication, condemning HIV-positive patients to a life of continuous health deterioration. · Kenya’s Anti-Counterfeit Act could be interpreted to preclude genuine generic antiretroviral therapy to more affordably treat HIV infections. By enacting this legislation, the government violated its duty to ensure people have access to the medicines they need to stay healthy. |
| Human Rights Standards | Treaty Body Interpretation |
| UDHR 25(1): Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including … medical care | |
| ICESCR 12(1): The States Parties to the present Covenant recognize the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. |
CESCR General Comment 14: Affirming “[m]ore determinants of health are being taken into consideration, such as resource distribution and that “formerly unknown diseases, such as human immunodeficiency virus and acquired immunodeficiency syndrome (HIV/AIDS), and others that have become more widespread, such as cancer, as well as the rapid growth of the world population, have created new obstacles for the realization of the right to health which need to be taken into account.” Para. 10 (2000). CESCR General Comment 14: Concerning economic accessibility (affordability): “health facilities, goods and services must be affordable for all. Payment for health-care services, as well as services related to the underlying determinants of health, has to be based on the principle of equity, ensuring that these services, whether privately or publicly provided, are affordable for all, including socially disadvantaged groups. Equity demands that poorer households should not be disproportionately burdened with health expenses as compared to richer households. Para. 12b (2000). CESCR General Comment 14: On the right to prevention, treatment and control of diseases, affirming the importance of “goods and services” that are “scientifically and medically appropriate and of good quality. This requires, inter alia….scientifically approved and unexpired drugs.” “The control of diseases refers to… the implementation or enhancement of immunization programmes and other strategies of infectious disease control.” Para 12.2c (2000). CESCR General Comment 14: Indicating that access to “essential drugs, as defined by the WHO Action Programme on Essential Drugs” is part of the minimum core content of the right to health. Fourteen palliative care medications are currently on the WHO Essential Drug List. Para. 43, (2000). |
| ADRDM 6 Every person has the right to the preservation of his health through sanitary and social measures relating to food, clothing, housing and medical care, to the extent permitted by public and community resources. |
| Human Rights Standards | Case Law |
| Constitution of Argentina, and Article 11 of the American Declaration of the Rights and Duties of Man, Article 25 of the UDHR, and Article 12 of the ICESCR, all of which have attained constitutional legal status in Argentina. | Federal Administrative Court of Appeals of Argentina: Court ordered the government to complete an unfinalized project to produce and distribute the vaccine for the Argentine Hemorrhagic Fever in order to comply with its national and international obligations regarding the right of health. Viceconte, Mariela Cecilia v. Argentine Ministry of Health and Social Welfare. Case n° 31. 777/96 (1998). |
| Constitution of Brazil 196: Health is a right of all and a duty of the State and shall be guaranteed by means of social and economic policies aimed at reducing the risk of illness and other hazards and at the universal and equal access to actions and services for its promotion, protection and recovery. | Federal Supreme Court of Brazil: Finding that the federal and state governments were responsible for the provision and distribution of essential medicines to needy populations (including those with the inability to pay for the required medications and those suffering from HIV/AIDS), under the responsibility set out by the constitutional right to health. State of Pernambuco v. Geni Lira de Sales. AI 676044/PE (2007). |
| Other Interpretations |
|
WHO 1946 Constitution: “The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition” and “Unequal development in different countries in the promotion of health and the control of disease, especially communicable disease, is a common danger.” [OHCRH website] SR Health: However, many countries have failed to adapt their drug control systems to ensure adequate medication supply; those systems were often enacted before contemporary treatment methods for chronic pain and drug dependence were known or devised. That constitutes an ongoing infringement of the right to health, as the Committee on Economic, Social and Cultural Rights has elaborated that access to essential medicines is a minimum core obligation of the right, and States must comply immediately with this non-derogable obligation regardless of resource constraints. A/65/255 (August 6, 2010). SR Health: “The failure to ensure access to controlled medications for pain and suffering threatens fundamental rights to health and to protection against cruel, inhuman and degrading treatment.” Banjul Charter, Art. 16: “Every individual shall have the right to enjoy the best attainable state of physical and mental health.” European Social Charter, Art. 11(3): Contracting parties should undertake “appropriate measures designed inter alia . . . to prevent as far as possible epidemic, endemic and other diseases.” European Social Charter, Art., 13(1): Contracting parties should undertake “to ensure that any person who is without adequate resources and who is unable to secure such resources . . . be granted adequate assistance, and, in case of sickness, the care necessitated by his condition.” |
Table 4: Access to Medicines and the Right to Enjoy the Benefits of Scientific Progress and its Applications
| Examples of Human Rights Violations |
|
· With one of the highest rates of hepatitis C infection in Europe, Romanians know all too well that the standard treatment has limitations and a variety of side effects. New hope came when the novel wonder drug, sofosbuvir (Sovaldi®) was hailed to virtually cure Hepatitis C. But with a price tag of $50,000 per 12 week treatment, it is far out of reach for the Romanian government and patients. · Several neglected tropical diseases (NTD) caused by parasites, such as lymphatic filariasis or chistosomiasis, can be stopped through preventative chemotherapy. Recently, targeted populations have benefited from chemotherapy, yet Indonesia, Nigeria, Ethiopia the Democratic Republic of Congo and Tanzania still have large populations in need of access to at least one NTD treatment. |
| Human Rights Standards | Treaty Body Interpretation |
| UDHR 27(1) Everyone has the right freely to participate in the cultural life of the community, to enjoy the arts and to share in scientific advancement and its benefits. | |
| ICESCR 15(1)(b) The States Parties to the present Covenant recognize the right of everyone… [t]o enjoy the benefits of scientific progress and its applications… |
| Human Rights Standards | Case Law |
| ICESCR 15: 1. The States Parties to the present Covenant recognize the right of everyone: (b) To enjoy the benefits of scientific progress and its applications. |
Constitutional Court of Venezuela: Finding that although there is no express right to benefit from scientific and technological advances in the Venezuelan Constitution, and citing to this right under the ICESCR, the denial of lack of access to HIV medicines and testing services by the Venezuelan Social Security Institute violated this right, as well as the right to life and the right to health. López, Glenda & Ors. v. Instituto Venezolano de los Seguros Sociales (IVSS). Expediente No. 00-1343, Sentencia No. 487 (2001).
|
| Other Interpretations |
|
SR Cultural Rights (2012): Para. 61. The Special Rapporteur notes that new incentives have been proposed to ensure innovation and access to medicines at affordable costs, in particular for those living in extreme poverty. Importantly, the WTO Doha Declaration on the TRIPS Agreement and public health explicitly recognizes that the TRIPS Agreement “can and should be interpreted and implemented in a manner supportive of WTO Members’ right to protect public health”, and reaffirmed the right to use the flexibilities included in the Agreement for this purpose. A/HRC/20/26 (2012). Statement of the Committee on Economic, Social and Cultural Rights (Committee on Economic, Social and Cultural Rights, Human Rights and Intellectual Property, 2001): [T]he Committee draws attention to the various intellectual property treaties administered by the World Intellectual Property Organization (WIPO), as well as the Agreement on Trade-Related Aspects of Intellectual Property Rights (the TRIPS Agreement) of the World Trade Organization (WTO), which set out minimum standards for the protection and enforcement of intellectual property rights. Reference could also be made to relevant articles of other treaties, such as the 1992 Convention on Biological Diversity…. [T]he Committee recalls previous statements it has made in which it emphasized that the realms of trade, finance and investment are in no way exempt from human rights principles and that “international organizations with specific responsibilities in those areas should play a positive and constructive role in relation to human rights.” E/C.12/2001/15 (2001). Protocol San Salvador 14(1b) The States Parties to this Protocol recognize the right of everyone… [t]o enjoy the benefits of scientific and technological progress. Access to medication in the context of pandemics such as HIV/AIDS, tuberculosis and malaria, Resolutions 2005/23, 2004/26, 2003/29 & 2002/32 (UN Commission on Human Rights). General Comment No. 17: The right of everyone to benefit from the protection of the moral and material interests resulting from any scientific, literary or artistic production of which he is the author (art. 15 (1) (c)) (CESCR, 2006): States parties should ensure that their intellectual property regimes constitute no impediment of their ability to comply with their core obligations in relation to the right to health … States thus have a duty to prevent that unreasonably high license fees or royalties for access to essential medicines … undermine the right … of large segments of the population to health …. E/C.12/GC/17 (2006). Political Declaration on HIV/AIDS (UN General Assembly, 2006): Para. 33. Emphasize the need for accelerated scale-up of collaborative activities on tuberculosis and HIV, in line with the Global Plan to Stop TB 2006–2015, and for investment in new drugs, diagnostics and vaccines that are appropriate for people with TB-HIV co-infection. Abuja Call for Accelerated Action Towards Universal Access to HIV/AIDS, Tuberculosis and Malaria Services in Africa (African Union, 2006): Research and Development. To promote and support research and development of microbicides, vaccines, diagnostics and treatment for HIV and AIDS, TB and malaria, including traditional medicine. Sp/Assembly/ATM/2 (I) Rev.3 (2006). Doha Declaration on the TRIPS Agreement and Public Health (World Trade Organization, 2001): Para. 4. [T]he TRIPS Agreement does not and should not prevent members from taking measures to protect public health. Accordingly, while reiterating our commitment to the TRIPS Agreement, we affirm that the Agreement can and should be interpreted and implemented in a manner supportive of WTO members’ right to protect public health and, in particular, to promote access to medicines for all. WT/MIN(01)/DEC/2 (2001).
|
Table 5: Access to Medicines and the Rights of Children
| Examples of Human Rights Violations |
|
· Meningitis, an infectious disease that causes the lining around the brain and spinal cord to swell, was endemic in certain regions of Colombia. Children lacking immunity and living in impoverished conditions where the disease can rapidly spread are at higher risk of infection. The meningitis vaccine was priced beyond the means of the poor families residing in the affected areas and was not provided as part of the government’s standard nor extended immunisation programmes. · Most medicines are produced in sizes and dosages fit for adults. Child sized medicines adapted to their smaller weight and palate are lacking, especially for tuberculosis where tablets are notoriously large, bitter tasting and difficult to swallow. Carers may even have to crush or chop adult pills for children to use, with little certainty that young patients are receiving the correct dose. |
| Human Rights Standards | Treaty Body Interpretation |
|
ICESCR (12a) The steps to be taken by the States Parties to the present Covenant to achieve the full realization of this right shall include those necessary for: (a) The provision for the reduction of the stillbirth-rate and of infant mortality and for the healthy development of the child. |
CESCR, General Comment 14(14): “The provision for the reduction of the stillbirth rate and of infant mortality and for the healthy development of the child” (Art. 12.2 (a)) may be understood as requiring measures to improve child and maternal health, sexual and reproductive health services, including access to family planning, pre- and post-natal care, emergency obstetric services and access to information, as well as to resources necessary to act on that information. E/C.12/2000/4 (August 11, 2000). CESCR, General Comment 14(52): Violations of the obligation to fulfill occur through the failure of States parties to take all necessary steps to ensure the realization of the right to health. Examples include the failure . . . to reduce infant and maternal mortality rates. E/C.12/2000/4 (August 11, 2000). CESCR: Expressing concern over high maternal, infant and under-five mortality rates in Angola E/C.12/AGO/CO/3 (CESCR, 2009), para. 36; Democratic Republic of Congo E/C.12/COD/CO/4 (CESCR, 2009) para. 34; Kenya E/C.12/KEN/CO/1 (CESCR, 2008) para. 32; and Morocco E/C.12/1/ADD.55 (CESCR, 2000), para. 29. CESCR: Recommending that Benin “step up its efforts to prevent and halt killings of so-called “witch children” by including provisions in criminal law to suppress this practice and organizing campaigns to heighten awareness of its criminal nature among local authorities, doctors, midwives and the population at large.” E/C.12/BEN/CO/2 (CESCR, 2008), para. 40. |
| CRC 6 States Parties recognize that every child has the inherent right to life … States Parties shall ensure to the maximum extent possible the survival and development of the child. | |
| CRC 24(1) States Parties recognize the right of the child to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and rehabilitation of health. States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services. |
CRC, General Comment 15 (2013) on the right of the child to the enjoyment of the highest attainable standard of health (art. 24): States have an obligation to make all essential medicines on the World Health Organization Model Lists of Essential Medicines, including the list for children (in paediatric formulations where possible) available, accessible and affordable. CRC: Expressing concern to Portugal that “Infant mortality, under-5 mortality and child tuberculosis rates remain higher than the regional average, particularly in some northern rural areas, and are also too high in the Azores” and recommending that the State “[i]ncrease investment in public health care facilities, including investments by civil society” and “[e]nsure the equal access of all children to the highest attainable standard of health care in all areas of the country.” CRC/C/15/Add.162 (2001). CRC: Expressing concern to Uzbekistan “at the increasing number of children infected with preventable diseases, such as Tuberculosis …” and recommending that the State “[c]ontinue its reform of the health sector and its efforts to strengthen the primary care centres and the preventive health services.” CRC/C/UZB/CO/2 (2006). CRC: Expressing concern in Armenia about “the continuous growth in tuberculosis morbidity among children” and recommending that the government “[t]ake measures to reduce child and infant mortality rates and combat tuberculosis.” CRC/C/15/Add.225 (2004). CRC: Expressing concern Gabon that it continues “to be threatened by early childhood diseases such as … tuberculosis” and recommending that it “[r]einforce its efforts to allocate appropriate resources and develop and implement comprehensive policies and programmes to improve the health situation of children, particularly in rural areas” and “[f]acilitate greater access to primary health service.” CRC/C/15/Add.171 (2002). CRC: Expressing concern to Uzbekistan at the “high incidence of infectious diseases, such as tuberculosis, despite high rates of immunization” and recommending the State “[i]mplement the 2000 Amsterdam Declaration to Stop TB.” CRC/C/15/Add.167 (2001). CRC: Expressing concern to Ethiopia “at the high incidence of malaria and tuberculosis and their effects upon children, at the fragile health infrastructure, limited health awareness among the public and the limited implementation of the 1993 Health Policy and the 1994 Social Policy” and urging the State to “ensure that access to primary health care services is increased, that national health infrastructure is strengthened and that public health education programmes are used to lower infant mortality rates and raise life expectancy in the State party.” CRC/C/15/Add.144 (2001). CRC: Expressing concern to Lithuania “at the high rates of child morbidity, in particular the increase in cases of tuberculosis” and recommending that the State “allocate appropriate resources and develop comprehensive policies and programmes to improve the health situation of all children.” CRC/C/15/Add.146 (2001). CRC: Noting that Mauritania has a “resurgence of tuberculosis” and recommending that the State “[a]llocate appropriate resources and develop comprehensive policies and programmes to improve the health situation of all children without discrimination, in particular by focusing more on primary care and further decentralizing the health care system.” CRC/C/15/ADD.159 (2001). CRC: Noting that Moldova has a “high incidence of tuberculosis … in schoolchildren” and recommending that the State “[d]efine sustainable financing mechanisms for the health care system, including adequate salaries for child health care professionals, in order to ensure that all children, in particular children from the most vulnerable groups, have access to free basic health care of good quality.” CRC/C/15/Add.192 (2002). |
| Human Rights Standards | Case Law |
| Constitution of Colombia: The following are basic rights of children: life, physical integrity, health and social security, a balanced diet, their name and citizenship, to have a family and not be separated from it, care and love, instruction and culture, recreation, and the free expression of their opinions. They will be protected against all forms of abandonment, physical or moral violence, imprisonment, sale, sexual abuse, work or economic exploitation, and dangerous work. They will also enjoy other rights upheld in the Constitution, the laws, and international treaties ratified by Colombia. | Colombian Constitutional Court: Finding violations of the right to life, to health, and to social security of children in the failure of the government to provide free, available meningitis vaccinations to children in a low-income sector of Bogota. Case SU-225/98 (1998). |
|
Right to health, right to life, and rights of the child as expressed in international human rights treaties ratified by Argentina and considered to have constitutional legal status.
|
Supreme Court of Argentina: Holding that the National Bank of Antineoplastic Drugs halting the provision of free Neutromax 300 – a drug on which a child with severe bone marrow defect was entirely dependent – was unconstitutional and that the federal state had the duty to provide medicines because of its international and constitutional responsibilities. Campodónico de Beviacqua, Ana Carina v. Ministerio de Salud y Acción Social – Secretaría de Programas de Salud y Banco de Drogas Neoplásicas. C. 823. XXXV (2000). |
| Other Interpretations |
|
WHO Model List of Essential Medicines, Children (WHO, 2011). South Africa: The South African Court established that “[the children’s] needs are ‘most urgent’ and their inability to have access to Nevirapine profoundly affects their ability to enjoy all rights to which they are entitled. Their rights are ‘most in peril’ as a result of a policy that has been adopted and are most affected by a rigid and inflexible policy that excludes them from having access to Nevirapine.” CRC, General Comment 3 (2003) (art. 25): The obligations of States parties under the Convention extend to ensuring that children have sustained and equal access to comprehensive treatment and care, including necessary HIV-related drugs . . . It is now widely recognized that comprehensive treatment and care includes anti-retroviral and other drugs, diagnostics and related technologies for the care of HIV/AIDS, related opportunistic infections and other conditions ….CRC/GC/2003/1 (2003). WHO Guidance on ethics of tuberculosis prevention, care and control (WHO, 2010): The obligation to provide access to TB services. Interventions should be gender-sensitive and address different types of vulnerabilities…. In addition, the needs of women, children, and people coinfected with HIV warrant special consideration. WHO Guidelines for the programmatic management of drug-resistant tuberculosis: Emergency Update (WHO, 2008): Extensive discussion of TB prevention, treatment and care options for children. Select recommendations: 9.5 Children. …Anecdotal evidence suggests that adolescents are at high risk for poor treatment outcomes. Early diagnosis, strong social support, individual and family counselling and a close relationship with the medical provider may help to improve outcomes in this group. WHO Guidance for national tuberculosis programmes on the management of tuberculosis in children (WHO, 2006). Abuja Call for Accelerated Action Towards Universal Access to HIV/AIDS, Tuberculosis and Malaria Services in Africa (African Union, 2006): Protection of Human Rights. To continue promoting an enabling policy, legal and social environment that promotes human rights particularly for women, youth and children and ensure the protection of people infected and affected by HIV and AIDS, TB and Malaria…. Prevention, Treatment, Care and Support. To invest heavily in evidence-based prevention as the most cost-effective intervention with focus on young people, women, girls and other vulnerable groups. Sp/Assembly/ATM/2 (I) Rev.3 (2006). Patients’ Charter for Tuberculosis Care (World Care Council, 2006): Care. The right to free and equitable access to tuberculosis care, from diagnosis through treatment completion, regardless of resources, race, gender, age, language, legal status, religious beliefs, sexual orientation, culture, or having another illness. |
Table 6: Access to Medicines and the Rights of Women
| Examples of Human Rights Violations |
| · Incorrect information circulated in Colombia by the Attorney General about how contraception containing levonorgestrel functioned, suggesting it is akin to an abortifacient and consequently illegal in the country. Empowering women to control their reproduction and engage in family planning relies on access to accurate information about contraception. |
| Human Rights Standards | Treaty Body Interpretation |
| CEDAW 12(1) States Parties shall take all appropriate measures to eliminate discrimination against women in the field of health care in order to ensure, on a basis of equality of men and women, access to health care services, including those related to family planning. |
CEDAW: Recommending that Kyrgyzstan “strengthen measures to reduce … the spread of tuberculosis and other diseases among women.” CEDAW/C/KGZ/CO/3 (2008). CEDAW: Expressing concern to the increase of tuberculosis among women to Estonia A/57/38(SUPP) (2002), Vietnam A/56/38(SUPP) (2001), and Lithuania A/55/38(SUPP) (2000). CEDAW Committee General Recommendation No. 24 (18): explaining that “[t]he issues of HIV/AIDS and other sexually transmitted diseases are central to the rights of women and adolescent girls to sexual health. Adolescent girls and women in many countries lack adequate access to information and services necessary to ensure sexual health… States parties should ensure, without prejudice or discrimination, the right to sexual health information, education and services for all women and girls…”
|
| Human Rights Standards | Case Law |
| Constitution of South Africa 27: 1. Everyone has the right to have access to – (a) health care services, including reproductive health care; . . . 2. The state must take reasonable legislative and other measures, within its available resources, to achieve the progressive realization of each of these rights. | Constitutional Court of South Africa: Holding that the Government’s restriction preventing the provision of the drug Nevirapine to prevent the transmission of HIV from mothers to infants during childbirth in public hospitals and clinics was unconstitutional. Additionally, it called for a reformulation of the policy that provided this medicine at certain pilot-sties to increase availability and to “meet the constitutional requirement of providing reasonable measures within available resources for the progressive realisation of the rights of such women and newborn children.” Minister of Health v. Treatment Action Campaign (No. 2). ZACC 15; 2002 (5) SA 721; 2002 (10) BCLR 1033. |
| Other Interpretations |
|
Declaration of Commitment of HIV/AIDS: By 2005, implement measures to increase capacities of women and adolescent girls to protect themselves from the risk of HIV infection, principally through the provision of health care and health services, including for sexual and reproductive health, and through prevention education that promotes gender equality within a culturally and gender-sensitive framework. Beijing Platform for Action – Women and health: Women have the right to the enjoyment of the highest attainable standard of physical and mental health. The enjoyment of this right is vital to their life and well-being and their ability to participate in all areas of public and private life. UN Commission on the Status of Women (2011): Calls on Governments to integrate HIV prevention, voluntary counselling and voluntary testing of HIV into other health services, including sexual and reproductive health, family planning, maternity and tuberculosis services. Resolution 55/2 (2011). Women’s health in prison: Action guidance and checklists to review current policies and practices (WHO, UNODC, 2011): Para. 1. The underlying importance of human rights should underpin all thinking and all policy development for all those in compulsory detention. Para. 3. Key services to be provided should include… specialist health care, which is readily provided and adjusted to meet the needs of women, such as for… chronic health conditions, HIV and AIDS (including counselling and support), hepatitis, tuberculosis (TB) and other infectious diseases…. WHO Guidance on ethics of tuberculosis prevention, care and control (WHO, 2010): The obligation to provide access to TB services. Interventions should be gender-sensitive and address different types of vulnerabilities…. In addition, the needs of women, children, and people coinfected with HIV warrant special consideration. Agreed Conclusions of the Commission on the Status of Women on the Critical Areas of Concern of the Beijing Platform for Action 1996-2009 (UN DESA, 2010): Recommending that governments, the UN system and civil society undertake measures to: “[i]ncrease the preventive, as well as the therapeutic, measures against tuberculosis and malaria”; intensify “support of national efforts against HIV/AIDS, particularly in favour of women and young girls, including efforts to provide affordable antiretroviral drugs, diagnostics and drugs to treat tuberculosis and other opportunistic infections”; “incorporate gender perspectives and human rights in health-sector policies and programmes”; and “recognize that the lack of economic empowerment and independence increased women’s vulnerability to a range of negative consequences, involving the risk of contracting HIV/AIDS, malaria, tuberculosis and other poverty-related diseases” ST/ESA/327 (2010). Resolution WHA 62.15, Prevention and control of multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis (WHO, 2009): Para. 4. Urging member states “to increase investment by countries and all partners substantially in operational research and research and development for new diagnostics, medicines and vaccines to prevent and manage tuberculosis including multidrug-resistant and extensively drug-resistant tuberculosis”. Resolution WHA 62.15. Beijing Call for Action on Tuberculosis control and patient care: together addressing the global MDR-TB and XDR-TB epidemic (WHO, 2009): Para. 1(i). …[S]upporting developing countries to establish manufacturing plants to produce combined preparations of anti-TB medicines … to ensure adequate drug supply for the prevention and control of M/XDR-TB. WHO Guidelines for the programmatic management of drug-resistant tuberculosis: Emergency Update (WHO, 2008): Extensive discussion of TB prevention, treatment and care options for women. Select recommendations: 9.2 Pregnancy. All female patients of childbearing age should be tested for pregnancy upon initial evaluation…. [B]irth control is strongly recommended for all non-pregnant women receiving therapy for DR-TB because of the potential consequences for both mother and fetus resulting from frequent and severe adverse drug reactions. Pregnant patients should be carefully evaluated, taking into consideration gestational age and severity of the DR-TB. 9.3 Breastfeeding. A woman who is breastfeeding and has active DR-TB should receive a full course of antituberculosis treatment. 11.2 Pretreatment screening and evaluation. Methods of avoiding pregnancy during treatment for women of childbearing age should be discussed. SR Health (2006): Commenting in Uganda, “stigma related to tuberculosis can be greater for women: it may lead, inter alia, to ostracism, rejection and abandonment by family and friends, as well as loss of social and economic support”. E/CN.4/2006/48/Add.2 (2006) Patients’ Charter for Tuberculosis Care (World Care Council, 2006): Care. The right to free and equitable access to tuberculosis care, from diagnosis through treatment completion, regardless of resources, race, gender, age, language, legal status, religious beliefs, sexual orientation, culture, or having another illness. Abuja Call for Accelerated Action Towards Universal Access to HIV/AIDS, Tuberculosis and Malaria Services in Africa (African Union, 2006): Protection of Human Rights. To continue promoting an enabling policy, legal and social environment that promotes human rights particularly for women, youth and children and ensure the protection of people infected and affected by HIV and AIDS, TB and Malaria…. Prevention, Treatment, Care and Support. To invest heavily in evidence-based prevention as the most cost-effective intervention with focus on young people, women, girls and other vulnerable groups. Sp/Assembly/ATM/2 (I) Rev.3 (2006). Gender and tuberculosis control: towards a strategy for research and action (WHO, 1999). Noting that research strategies are needed to “[d]evelop guidelines and tools for TB programmes to minimise gender disparities”. Beijing Declaration and Platform for Action (UN, 1995): 89. Women have different and unequal access to and use of basic health resources, including primary health services for the prevention and treatment of … tuberculosis, among others. |
Table 7: Access to Medicines and Freedom from Torture and Cruel, Inhuman, and Degrading Treatment
| Examples of Human Rights Violations |
|
| Human Rights Standards | Treaty Body Interpretation |
| UDHR 5 No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment. | |
| ICCPR 7 No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment. In particular, no one shall be subjected without his free consent to medical or scientific experimentation. | |
| ICCPR 10(1) All persons deprived of their liberty shall be treated with humanity and with respect for the inherent dignity of the human person | HRC: Article 10, paragraph 1, imposes on States parties a positive obligation towards persons who are particularly vulnerable because of their status as persons deprived of liberty, and complements for them the ban on torture or other cruel, inhuman or degrading treatment or punishment contained in article 7 of the Covenant. Thus, not only may persons deprived of their liberty not be subjected to treatment that is contrary to article 7, including medical or scientific experimentation, but neither may they be subjected to any hardship or constraint other than that resulting from the deprivation of liberty; respect for the dignity of such persons must be guaranteed under the same conditions as for that of free persons. HRI/GEN/1/Rev.9 (Vol. I) (1992). General Comment 21. |
| CRC 37(a) No child shall be subjected to torture or other cruel, inhuman or degrading treatment or punishment. Neither capital punishment nor life imprisonment without possibility of release shall be imposed for offences committed by persons below eighteen years of age. | |
|
CRC 39 States Parties shall take all appropriate measures to promote physical and psychological recovery and social reintegration of a child victim of: any form of neglect, exploitation, or abuse: torture or any other form of cruel, inhuman or degrading treatment or punishment; or armed conflicts. Such recovery and reintegration shall take place in an environment which fosters the health, self-respect and dignity of the child.
|
CRC, General Comment 8 (2006) on the right of the child to protection from corporal punishment and other cruel or degrading forms of punishment: “Corporal punishment and other degrading forms of punishment may inflict serious damage to the physical, psychological and social development of children, requiring appropriate health and other care and treatment. This must take place in an environment that fosters the integral health, self-respect and dignity of the child, and be extended as appropriate to the child’s family group.”
|
| CRPD 15 No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment. In particular, no one shall be subjected without his or her free consent to medical or scientific experimentation. 2. States Parties shall take all effective legislative, administrative, judicial or other measures to prevent persons with disabilities, on an equal basis with others, from being subjected to torture or cruel, inhuman or degrading treatment or punishment. |
| Human Rights Standards | Case Law |
| ECHR 3: No one shall be subjected to torture or to inhuman or degrading treatment of punishment. | ECtHR: Holding that the provision of only two medicines to a prisoner requiring three different medicines for tuberculosis lead to “prolonged mental and physical suffering diminishing his human dignity,” and this amounted to inhuman and degrading treatment. Gladkiy v. Russia, App. No. 3242/03, Eur. Ct. H.R. (2010). |
| ECHR 3: No one shall be subjected to torture or to inhuman or degrading treatment of punishment. | ECtHR: Finding that the removal of an HIV-positive St. Kitts national from the U.K. after imprisonment would amount to inhuman treatment as “his removal would expose him to a real risk of dying under most distressing circumstances”. The Court bases this decision on the exceptional circumstances of the critical stage of his illness and the impossibility of accessing the drugs needed for his treatment in St. Kitts. D v. United Kingdom, App. No. 30240/96, 24 Eur. H.R. Rep. 423 (1997). |
| United States Constitution, Amendment 8: Excessive bail shall not be required, nor excessive fines imposed, nor cruel and unusual punishments inflicted. | 11th Circuit Court of Appeals of the United States: Holding that stopping to prescribe medications to a prisoner suffering from HIV and hepatitis was a violation of the Eighth Amendment because of the seriousness of the medical needs of the patient, and the deliberate indifference to these needs by the doctors and the prison. Brown v. Johnson, 387 F.3d 1344 (2004). |
| Other Interpretations |
|
SR Torture and Other Cruel, Inhuman, or Degrading Treatment or Punishment “Ensuring the availability and accessibility of medications included in the WHO Model List of Essential Medicines is not just a reasonable step but a legal obligation under the Single Convention on Narcotic Drugs, 1961. When the failure of States to take positive steps, or to refrain from interfering with health-care services, condemns patients to unnecessary suffering from pain, States not only fall foul of the right to health but may also violate an affirmative obligation under the prohibition of torture and ill-treatment (A/HCR/10/44 and Corr.1, para. 72). In a statement issued jointly with the Special Rapporteur on the right to health, the Special Rapporteur on the question of torture reaffirmed that the failure to ensure access to controlled medicines for the relief of pain and suffering threatens fundamental rights to health and to protection against cruel, inhuman and degrading treatment. Governments must guarantee essential medicines – which include, among others, opioid analgesics – as part of their minimum core obligations under the right to health, and take measures to protect people under their jurisdiction from inhuman and degrading treatment.” Para. 55 & 56 A/HRC/22/53 (2013)
Economic and Social Council: “The right to health contains both freedoms and entitlements. The freedoms include the right to control one’s health and body, including sexual and reproductive freedom, and the right to be free from interference, such as the right to be free from torture, non-consensual medical treatment and experimentation.” Para. 8 E/C/2000/4 |
What is a human rights-based approach to advocacy, litigation, and programming?
What is a human rights-based approach?
“Human rights are conceived as tools that allow people to live lives of dignity, to be free and equal citizens, to exercise meaningful choices, and to pursue their life plans.”[174]
A human rights-based approach (HRBA) is a conceptual framework that can be applied to advocacy, litigation, and programming and is explicitly shaped by international human rights law. This approach can be integrated into a broad range of program areas, including health, education, law, governance, employment, and social and economic security. While there is no one definition or model of a HRBA, the United Nations has articulated several common principles to guide the mainstreaming of human rights into program and advocacy work:
- The integration of human rights law and principles should be visible in all work, and the aim of all programs and activities should be to contribute directly to the realization of one or more human rights.
- Human rights principles include: “universality and inalienability; indivisibility; interdependence and interrelatedness; non-discrimination and equality; participation and inclusion; accountability and the rule of law.”[175] They should inform all stages of programming and advocacy work, including assessment, design and planning, implementation, monitoring and evaluation.
- Human rights principles should also be embodied in the processes of work to strengthen rights-related outcomes. Participation and transparency should be incorporated at all stages and all actors must be accountable for their participation.
A HRBA specifically calls for human rights to guide relationships between rights-holders (individuals and groups with rights) and the duty-bearers (actors with an obligation to fulfill those rights, such as States).[176] With respect to programming, this requires “[a]ssessment and analysis in order to identify the human rights claims of rights-holders and the corresponding human rights obligations of duty-bearers as well as the immediate, underlying, and structural causes of the non-realization of rights.”[177]
A HRBA is intended to strengthen the capacities of rights-holders to claims their entitlements and to enable duty-bearers to meet their obligations, as defined by international human rights law. A HRBA also draws attention to marginalized, disadvantaged and excluded populations, ensuring that they are considered both rights-holders and duty-bearers, and endowing all populations with the ability to participate in the process and outcomes.
What are key elements of a human rights-based approach?
Human rights standards and principles derived from international human rights instrument should guide the process and outcomes of advocacy and programming. The list below contains several principles and questions that may guide organisations in considering the strength and efficacy of human rights within their own programs or advocacy work. Together these principles form the acronym PANELS.
- Participation: Does the activity include participation by all stakeholders, including affected communities, civil society, and marginalized, disadvantaged or excluded groups? Is it situated in close proximity to its intended beneficiaries? Is participation both a means and a goal of the program?
- Accountability: Does the activity identify both the entitlements of claim-holders and the obligations of duty-bearers? Does it create mechanisms of accountability for violations of rights? Are all actors involved held accountable for their actions? Are both outcomes and processes monitored and evaluated?
- Non-discrimination: Does the activity identify who is most vulnerable, marginalized and excluded? Does it pay particular attention to the needs of vulnerable groups such as women, minorities, indigenous peoples, disabled persons and prisoners?
- Empowerment: Does the activity give its rights-holders the power, capacity, and access to bring about a change in their own lives? Does it place them at the center of the process rather than treating them as objects of charity?
- Linkage to rights: Does the activity define its objectives in terms of legally enforceable rights, with links to international, regional, and national laws? Does it address the full range of civil, political, economic, social, and cultural rights?
- Sustainability: Is the development process of the activity locally owned? Does it aim to reduce disparity? Does it include both top-down and bottom-up approaches? Does it identify immediate, underlying and root causes of problems? Does it include measurable goals and targets? Does it develop and strengthen strategic partnerships among stakeholders?
Why use a human rights-based approach?
There are many benefits to using a human rights-based approach to programming, litigation and advocacy. It lends legitimacy to the activity because a HRBA is based upon international law and accepted globally. A HRBA highlights marginalized and vulnerable populations. A HRBA is effective in reinforcing both human rights and public health objectives, particularly with respect to highly stigmatizing health issues.[178] Other benefits to implementing a human rights-based approach include:
- Participation: Increases and strengthens the participation of the local community.
- Accountability: Improves transparency and accountability.
- Non-discrimination: Reduces vulnerabilities by focusing on the most marginalized and excluded in society.
- Empowerment: Capacity building.
- Linkage to rights: Promotes the realization of human rights and greater impact on policy and practice.
- Sustainability: Promotes sustainable results and sustained change.
How can a human rights-based approach be used?
A variety of human rights standards at the international and regional levels applies to patient care. These standards can be used for many purposes including to:
- Document violations of the rights of patients and advocate for the cessation of these violations.
- Name and shame governments into addressing issues.
- Sue governments for violations of national human rights laws.
- File complaints with national, regional and international human rights bodies.
- Use human rights for strategic organizational development and situational analysis.
- Obtain recognition of the issue from non-governmental organizations, governments or international audiences. Recognition by the UN can offer credibility to an issue and move a government to take that issue more seriously.
- Form alliances with other activists and groups and develop networks.
- Organize and mobilize communities.
- Develop media campaigns.
- Push for law reform.
- Develop guidelines and standards.
- Conduct human rights training and capacity building
- Integrate legal services into health care to increase access to justice and to provide holistic care.
- Integrate a human rights approach in health services delivery.
4. What are some examples of effective human rights-based work in advancing access to medicines?
This section contains four examples of effective human rights-based work in the area of patient care and human rights. These are:
- Challenging the 2008 Anti-Counterfeit Act in Kenya
- Litigating to increase access to HIV drugs in India
- Promoting TRIPS flexibilities to increase access to medicines in Uganda
- Litigating for prisoners with Hepatitis C in Georgian prisons
Example 1: Challenging the 2008 Anti-Counterfeit Act in Kenya
Project Type
Advocacy/Litigation
Organization
Founded in 1994 and formally registered in 2001, KELIN is a national NGO in Kenya that responds to human rights concerns relating to health, including access to medicines.
AIDS Law Project Kenya (ALP) is a non-governmental organization that works to promote equal rights and justice for people living with HIV and AIDS. ALP employs legal strategies to advance health rights for people living with and affected by HIV and AIDS.[179]
Problem
The 2008 Anti-Counterfeit Act posed a threat for people living with HIV/AIDS in their pursuit of life-saving medicines. By failing to distinguish between counterfeit goods and generic medicines, the Act threatened to limit the availability and affordability of ARVs in Kenya. Since 90% of Kenyan patients with HIV depend on generic drugs imported by the government and donors, the Act’s potential repercussions could have been tremendous. On the whole, the incidence of HIV in Kenya is especially high, particularly for women and children. According to the 2010 Country Report to the United Nations General Assembly Special Session on HIV and AIDS, the National Aids Control Council, citing the Kenya AIDS Indicators Survey (2007), 7.4% of the population aged 15-49 is infected with HIV. 8.4% of women are infected compared to 5.4% of men. The Kenya National HIV and AIDS Estimates (2010) reports that mother-to-child transmission of HIV/AIDS makes children especially at risk.[180]
Actions Taken
On June 8, 2009, the firm of Majanja Luseno & Company Advocates filed a case on behalf of three adults living with HIV/AIDS, bringing on a constitutional challenge to the High Court of Kenya (the “Anti-Counterfeit Case”). Patricia Asero, Maurine Murenga, and Joseph Munyi had been taking HIV drugs for the last ten years or so since generic antiretroviral (ARV) HIV drugs became widely available as a result of the 2001 Industrial Property Act. The three applicants claimed that the Anti-Counterfeit Act of 2008 would deny them the opportunity to purchase generic drugs, substantially increasing the cost of HIV medication. AIDS Law Project Kenya (ALP) and the United Nations Special Rapporteur for Health, Anand Grover, were enjoined as interested parties to this case. KELIN provided research support to the lead advocate during the case.
Arguing that the Act amounted to a violation of their rights to life, dignity, and health, Asero, Murenga, and Munyi urged the government to consider the Act again and re-draft it as it related to the definition of counterfeit medicine. More specifically, the petitioners claimed that the Act, as written in section 2, failed to exempt generic medicines from its definition of “counterfeit goods,” which was referred to as:
“manufacture, production…or making, whether in Kenya or elsewhere, of any goods whereby those protected goods are imitated in such manner and to such a degree that those other goods are identical or substantially similar copies of the protected goods.”[181]
By neglecting to outline a clear distinction between both terms, the Act had the potential to prohibit the importation and manufacture of generic medicines in Kenya. The Act also outweighed the positive effects of the Industrial Property Act (2001) which had allowed for parallel importation of medicines put legitimately on the market elsewhere, making generic drugs affordable and available in Kenya.
Asero, Murenga, and Munyi argued that the withholding of generic medications, which are taken daily for survival, constituted a violation of the right to life as guaranteed in the Kenyan Constitution (which came into force in 2010, after the case had been filed). The Act also directly conflicted with the 2006 HIV and AIDS Prevention and Control Act, which recognized the “special status” of persons living with HIV and AIDS and granted these persons “full protection of their human rights and civil liberties.”
Later enjoined as an interested party, the United Nations Special Rapporteur for Health, Anand Grover, underscored that “legitimately produced” generic medicines had been conflated with goods that violate private intellectual rights. He emphasized that this conflation was “likely to have a serious adverse impact on the availability, affordability and accessibility of low-cost, high-quality medicines.” Grover envisaged a variety of scenarios including that medicines, deemed safe and effective by regulatory mechanisms, might be withheld at Kenyan checkpoints. He also predicted significant delays on imported generics and a drastic rise in the price of ARVs.
The adoption of similar regulations in other jurisdictions served a case in point to Grover’s argument. For example, both in the Netherlands and in Germany, after the passage of similar provisions as outlined in the Anti-Counterfeit Act, custom authorities had seized generic drugs for HIV, which were suspected to be counterfeits.
In 2012, three years after the Anti-Counterfeit Case was filed, the High Court of Kenya ruled that the 2008 Anti-Counterfeit Act violated the rights to life, human dignity, and health as protected by the Constitution of Kenya. Justice Mumbi’s ruling affirmed that the provisions within the Act – particularly sections 2, 32, and 34 which had construed “counterfeit” products with generics – had impinged upon Kenyan patients’ access to affordable and essential drugs and medicines, thereby infringing upon their fundamental rights to life, human dignity and health as protected by the Constitution of Kenya and in international instruments ratified in line with Article 2(6) of the Constitution.[182]
Results and Lessons Learned
The outcome of the Anti-Counterfeit Case reaffirmed the rights of Kenyan patients living with HIV/AIDS and the obligation of the Kenyan government to fulfill its positive obligations towards them. In her ruling, Judge Mumbi Ngugi stated, “There can be no room for ambiguity where the right to health and life of the petitioners and the many other Kenyans who are affected by HIV/AIDS are at stake.”[183] The Anti-Counterfeit case resulted in the suspension of significant portions of the Anti-Counterfeit Act, in particular relating to parallel importation. The court also issued a directive commanding the amendment of sections 2, 32, and 34.[184] Finally, the Court referenced paragraph 35 of General Comment No. 17 of the CESCR, stating that
“[s]tates parties should prevent the use of scientific and technical progress for purposes contrary to human rights and dignity, including the rights to life, health and privacy, e.g. by excluding inventions from patentability whenever their commercialization would jeopardize the full realization of these rights.”[185]
Overall, the Anti-Counterfeit Case emphasized the importance of the right of the petitioners to access essential medicine over the protection of enforcing intellectual property rights. Moreover, it reaffirmed that the protection of consumers should not be a “collateral issue” in advancing the protection of intellectual property. The case has been deemed a milestone in the advancement of health and human rights in Kenya, and according to Allan Maleche, Executive Director of KELIN, it has since facilitated access to generic medicines for more than 430,000 people living with HIV in Kenya.
In addition to a strong litigation strategy on the part of KELIN and ALP, there were several other factors that contributed to the success of the litigation. For example, this case was particularly compelling because it coincided with the adoption of the Kenyan Constitution in 2010, which for the first time included the right to health. The recent codification of international human rights standards in Kenya’s national constitution also provided a robust discourse through which to advance justice in health. These constitutional changes importantly allowed the application of rights to health, dignity, and nondiscrimination, as enshrined within international human rights law, to drive arguments before the court. Once the petition was amended to reflect these constitutional changes in 2010, other key stakeholders, including the Special Rapporteur on the Right to Health, enjoined as interested parties.
In reflecting on the merits of the case, Maleche underscored the courage of the three Kenyans – Asero, Murenga, and Munyi – who bravely brought their testimonies before the court. Initially, the lawyers in the case had been poised to include several more testimonies in its application, but because of the entrenched stigma associated with HIV/AIDS in Kenya, several applicants withdrew their names. As such, the participation and bravery of Asero, Murenga, and Munyi in sharing their stories publicly was important and indispensable in advancing the case.
|
Additional Resources There are several resources to aide health right activists to understand the advances in right to health litigation and to help develop litigation strategies: B. M. Meier and A. E. Yamin, Right to Health Litigation and HIV/AIDS Policy, Journal of Law, Medicine & Ethics 39 (Spring 2011).
S. Gloppen, “Litigation as a Strategy to Hold Governments Accountable for Implementing the Right to Health,” Health and Human Rights 10/2 (2008), www.hhrjournal.org/index.php/hhr/article/viewFile/79/145. |
Contact Information:
KELIN
Nairobi, Kenya
Email: info@kelinkenya.org
Website: www.kelinkenya.org
Twitter: @KELINKenya
Facebook: KELIN
Youtube: KELIN Kenya
Example 2: Litigating to increase access to HIV drugs
Project Type
Litigation
The Organization
The Initiative for Medicines, Access & Knowledge (I-MAK) is a non-profit organization of lawyers and scientists representing the rights of low-income patients worldwide. The organization believes all people have the right to access affordable, life-saving medicines for HIV/AIDS and other diseases. I-MAK expands access to lower-cost generic medicines by addressing legal and policy barriers, focusing on challenging unmerited drug patents, conducting evidence-based research on drug pricing and patents, and conducting advocacy and law reform efforts to drive practice-based solutions to access problems.
Problem
In 2006, Lopinavir/ritonavir was considered the best drug combination available for patients who have failed HIV first line therapy.[186] Because the tablet form does not need to be refrigerated nor does it require adherence to a strict dietary regimen, it is particularly well suited to patients in resource-constrained settings.[187] However, access to Lopinavir/ritonavir was inhibited by Abbott Laboratories, the branded company that manufactured and sold the drug at the time. Abbott Laboratories, a major US pharmaceutical company, filed repeated requests to secure patents on various formulations of Lopinavir/ritonavir, a tactic that allowed Abbott to prolong exclusive rights over the combination and control the global market, setting the price out of reach for patients worldwide. A study of Abbott Laboratories patenting behaviour in the U.S. around Lopinavir/ritonavir showed that it had accumulated a total of 108 different granted patents and patent applications.[188]
Patient advocates, including I-MAK, deem pharmaceutical companies’ push to proliferate unjustified patents on essential drugs one of the biggest threats to people living with HIV. In this particular case, Abbot Laboratories filed a patent application with the Indian Patent Office and claimed its solid oral dosage formulation of Lopinavir/ritonavir—which had only been minimally modified—was “an invention.”
If Abbott had secured a patent over this Lopinavir/ritonavir formulation, the repercussions would have been grave: Namely, other companies in India would have been prohibited from manufacturing affordable generics, which in turn would have limited access to treatment for millions of patients who could not afford Abbott’s hefty price tag. At the time, Lopinavir/ritonavir cost $2200 per patient, per year as its middle-tier price, and $500 per patient, per year at its lowest price.
Since India was one of the leading suppliers of affordable generics to other low- and middle-income countries, a patented Lopinavir/ritonavir would have dramatically hampered access to treatment for many individuals in developing countries around the world beyond India.[189]
Actions Taken
On March 24th, 2006, Abbott Laboratories filed an application with the Indian Patent Office, claiming that its solid oral dosage formulation of Lopinavir/ritonavir amounted to an invention that would not be known or obvious to anyone skilled in the field. To satisfy the requirements of the Indian Patent Act, Abbott also claimed that the alleged new formulation possessed a significant enhancement of efficacy of the formulation already known.
In 2007, I-MAK filed a patent opposition against Abbott’s tablet patent application following three other patent oppositions I-MAK filed against Abbott on related patents that could also potentially block generic companies. I-MAK claimed that Abbott’s formulation in question was “not an invention that should be considered patentable within the meaning of the Act” and submitted a body of scientific/legal evidence to support its contention. I-MAK’s patent challenge also contended,
“[S]hould a patent be granted for the application in question, it will unfairly impede others from looking to develop and/or offer Lopinavir/ritonavir at more affordable prices. Moreover, it will contribute to preventing HIV patients from accessing this particular treatment at a cost they can afford.”[190]
I-MAK argued that in light of existing scientific knowledge and practices in the field, this tablet formulation lacked novelty and would have been obvious. I-MAK also argued that the formulation was a new form of a known substance that did not increase its efficacy over known forms. Therefore, it did not amount to an invention and was not patentable under the Act.
The Indian Patent Office Decision denied Abbott’s a patent on the grounds that the new formulation was not inventive. Importantly, I-MAK’s intervention in India allowed Indian companies to produce and distribute much cheaper generic versions of Lopinavir/ritonavir.
Abbott’s attempt to patent lopinavir/ritonavir was also contested in other parts of the world, either filed or supported by I-MAK. I-MAK was able to file multiple patent challenges with the European Patent Office (covering 38 countries) on Abbott’s patent applications around lopinavir/ritonavir. In the United States, the Public Patent Foundation filed patent challenges against ritonavir. In Brazil, NGO Rebrip’s Working Group on Intellectual Property filed a pre-grant patent challenge to Abbott’s application on the heat-stable versions of LPV/r and ritonavir.
According to Michelle Childs, former Director of Policy Advocacy of MSF Access Campaign, “Access to the drug lopinavir/ritonavir is critical for people living with HIV who have become resistant to their first medicine combination. Today we are concerned that access to this drug has shrunk with lopinavir/ritonavir now priced out of reach, which is quite worrying given the increasing number of people that need to switch to this drug.”[191]
Results and Lessons Learned
I-MAK’s challenge of Abbott’s patent applications was part of a larger scheme to reduce critical barriers to scaling up access to HIV treatment worldwide. “Abbott’s track record on pricing this drug unfairly for poorer countries motivated us to take on this case,” stated Tahir Amin, Director of I-MAK. “They have gamed the patent system for nearly twenty years to extend the patent life on this drug. The time has come to say, ‘enough is enough’.”
Facilitating the introduction of generics into the market is an important strategy in increasing access to medicines. According to I-MAK, cost-savings incurred over a three year period on just three HIV drugs – lopinavir/ritonavir, nevirapine and abacavir – generated a half billion dollars in cost savings, which can be re-invested in national health programs to put more people on treatment. Patent-legal interventions played a critical role in making lower-cost generic versions available globally.
“This groundbreaking victory for patients sets an important precedent to stop pharmaceutical companies from gaming the patent system, marking a new era of hope for millions of people living with HIV all over the world,” I-MAK wrote in a press release.[192]
|
Additional Resources Médecins Sans Frontières (MSF), Brazilians demand greater access to crucial HIV drug Civil society files patent opposition to increase access to HIV/AIDS medicines (2011), https://msfaccess.org/resources/press-releases/1682/ Indian Patent Office Decision (Application No. 339/MUMNP/2006) |
Contact Information:
I-MAK
Email: priti@i-mak.org (Director of Treatment Access)
Web: http://www.i-mak.org/
Example 3: Promoting TRIPS flexibilities to increase access to medicines
Project Type
Advocacy/ Law Reform
The Organization
The Center for Health, Human Rights and Development (CEHURD) is a health and human rights organization whose primary goal is enforce the realization of the right of health in Uganda. The organization empowers the community by making them aware of their rights inherent within the right to health. Working with government agencies and the Ministry of Health, CEHURD influences law and policy on the right to health, and through strategic litigation, provides pro bono legal services for those whose rights have been violated within the health system or neglected by the government.
The Problem
In Uganda, the prevalence of malaria, tuberculosis, and HIV/AIDS is high. However, Ugandans face steep barriers in their pursuit of medicines that treat these very diseases.[193] Many essential medicines are not available in government health facilities, and in the private sector, medicines are about 3-5 more expensive and unaffordable for most.[194] Though the price of ARV medications to treat HIV/AIDS has decreased in recent years, most Ugandans still cannot afford them.
CEHURD believes that the international trade regime has limited Uganda from realizing its obligation to respect the right to access medicines for its citizens. As this chapter has shown, strong IPR protection can drive up the prices of essential drugs and limit access to new medicines. Furthermore, certain provisions for patents under the TRIPS Agreement have prevented governments from addressing the public health needs of its citizens.
As a least developed country (LDC), Uganda has no obligation to implement patents for medicines. However, CEHURD is concerned that the government will not maximize full flexibilities under the TRIPS Agreement – thereby maximizing the right to health – within its draft national legislation. According to CEHURD, crucial gaps within the Industrial Properties Bill “are likely to prejudice Uganda’s interventions in making medicines affordable and accessible for most Ugandans after the 2016 patents enforcement deadline.”
Actions Taken
In anticipation of the 2016 patents enforcement deadline, CEHURD advocated for and worked with the government towards the inclusion of TRIPS flexibilities in the Industrial Property Bill of 2013.
To garner governmental support, CEHURD developed a policy brief addressing the Industrial Property Bill, which made the case for striking a balance between the public interests of access to medicines and the private interest of intellectual property protection. In the brief, CEHURD urged the Ugandan government, in reforming its intellectual property laws, to maximize public health benefits from the new IPR protection regime by “making the most” of all flexibilities within TRIPS and adopting only the minimum levels of IPR protection that the Agreement requires.
Furthermore, CEHURD warned that the bill’s current formulation contained unnecessary IPR protection “over and above” the minimum required by the TRIPS Agreement. Current legislation also failed to fully utilize flexibilities that address national public health crises or make use of the transition period to incorporate TRIPS, which least developed countries (LDCs) can take advantage of. CEHURD also encouraged bolstering the capacity at the national level for the production of generic medicines and allowing “the widest possible scope” for parallel importation. Finally, CEHURD encouraged the government to “adopt a simple and expeditious procedure for compulsory licensing and government use order; allow extensive flexibility for scientific research and regulatory approval exceptions (bolar/early working provisions); and disallow data exclusivity, i.e. allow the submitted data to be relied upon by authorities in assessing and granting approvals for supply of medicines.”
As part of its initiative to influence the Industrial Properties Bill, CEHURD hosted a convening with CSOs and Anand Grover, the then Special Rapporteur on the Right to Health, on issues affecting access to medicines in Uganda. CEHURD also developed a booklet outlining its recommendations and compiled a mailing list of key stakeholders to facilitate national discussion on the matter.
Complementing their work on the Industrial Properties Bill, CEHURD developed comprehensive written materials for journalists in an effort to help shape communications on how information about access to medicines is delivered to the public. Written in clear language with policymakers and program planners in mind, the pocketbook Intellectual Property and Human Rights, outlines the basic concepts of intellectual property and several related public interest issues, including access to medicines. The publication also highlights significant gaps in the legislation in promoting Uganda’s public health needs and identifies interventions that have been proven to work for achieving better access to medicines, thus providing the evidence base for those designing policies and programs. The handbook helps maximize the efficiency and effectiveness of HIV programs by providing, in one place, evidence of successful and promising approaches and interventions.
Intellectual Property and Human Rights is freely available online and in print for those with unreliable internet service, thus putting the evidence into the hands of those who cannot access or afford costly database subscriptions.
Lessons Learned
CEHURD’s policy brief on the Industrial Property Bill was the basis for advocating and working with the government towards the inclusions of TRIPS flexibilities in the Industrial Property Bill. CEHURD demonstrated that not only was it necessary to provide for pro-access to medicines provisions in form of flexibilities, but that pro-access provisions are permitted within the scope of the international obligations which Uganda has.
The Intellectual Property and Human Rights was used together with fellowships and calls for media stories through which media were trained and requested to document access to medicines stories in the context of the need for a pro-access to medicines Industrial Property Bill. The successful dissemination of the pocketbook suggests that, in advocating for increased access to essential medicines, the media is an important resource for generating public discussion and raising awareness about access to medicines issues. If well informed on the issue, the media can be used as a tool to raise awareness, generate public discourse, and convey accurate messaging that advance the public’s cause. As a resource, Intellectual Property and Human Rights can guide effective, evidence-based programming, and highlight what remains to be done to advance access to medicines.
Awareness of the full flexibilities under the TRIPS Agreement available to LDCs is only the first step. Identifying and implementing legislation that fully incorporates these allowances is the next step. Furthermore, when designing programs, policymakers and program planners have scarce resources and encounter a wide array of recommendations, best practices, scientific studies, and public health interventions. Policymakers and programmers have been forced, at best, to undertake their own research to identify effective programming and, at worst, to base policies and programs on unquestioned practices. Until now, there has not been one central location to obtain been a clear universal understanding in Uganda of clear methods to advance the highest attainable standard of health.
Contact Information:
CEHURD
Email: info@cehurd.org
Web: http://www.cehurd.org/
Example 4: Litigating for prisoners with Hepatitis C in Georgian prisons
Project Type
Litigation
Organization
The European Court of Human Rights
Open Society Georgia Foundation
Problem
Georgia has one of the highest rates of Hepatitis C incidence in the world (7%), only after Egypt and Mongolia.[195] The prevalence of the virus is especially high among populations infected with human immunodeficiency virus (HIV) (47%)[196] and injection drug users (50%–70%).[197] Before the change of government in 2012, HIV prevalence was also high among prisoners (50%).[198] Though prison conditions have since improved, a constellation of factors—including overcrowding, poor nutrition and sanitation, inadequate health care, and insufficient infection control measures—had previously made ground especially fertile for the spread of Hepatitis C.
Before the government’s intervention described in this case study, the steep price of the Hepatitis C drug, Pegylated-Interferon, had also made treatment a distant dream for many.[199] Out of 7% of the population infected with Hepatitis C, only 1% could afford the $18,000, 48-week course of treatment. Of prisoners, who depend on correctional facilities for their treatment, far fewer.[200] Though treatment of prisoners with Hepatitis C puts a financial strain on prison systems, this did not absolve the government from providing treatment. Even so, the excessive price tag of Pegylated-Interferon, patent-protected by the duopoly of Roche and Merck, proved a significant barrier for the Georgian government.[201]
Actions Taken
Poghosyan v. Georgia, which was brought before the European Court of Human Rights (ECtHR) in 2009, was the watershed event that pressured the Georgian government to make medicines available to Hepatitis C patients in prisons. The applicant, Khvicha Poghosyan from Bodbiskhevi, Georgia, argued that his right to protection from inhumane and degrading treatment had been violated under Article 3 of the European Convention on Human Rights. After receiving post-operative care in the prison hospital for a cystectomy, the plaintiff was transferred to Prison No. 6 in Rustavi, Georgia, where blood tests revealed that Poghosyan had contracted Hepatitis C. Upon learning of his condition, the prison staff failed to transfer Poghosyan to the prison hospital to access the necessary care. In response, Poghosyan’s attorney filed a complaint with the Governor of the prison. This request was repeatedly denied.
It is important to note the Poghosyan v. Georgia case was not unique. In fact, Poghosyan v. Georgia was one of several cases linked to the denial of medical care in Georgian prisons brought before the ECtHR. At the time, approximately half of these applications related to inadequate treatment of Hepatitis C for patients in prisons. As the ECtHR observed, these numbers suggested that “the problem of medical care in prisons, particularly care administered to detainees suffering from viral hepatitis C, inter alia, was a structural one.”[202]
The ECtHR ruled that the absence of Hepatitis C treatment in the prison constituted a violation of Article 3 (prohibition of inhuman or degrading treatment) for the applicant, who was infected with Hepatitis C. In the context of Article 46 (binding force and execution of judgments), the Court said that the state had to comply with the Court’s judgment and take necessary individual and general measures to remedy the violation.[203]
The ruling subsequently obliged Georgia to create a program targeting the prevention and treatment of HCV in prisons. The Court’s decision also motivated the Georgian government to negotiate the price of Hepatitis C treatment with its producer, Roche and Merk. Backed by civil society and patient groups, negotiations brought down the price of Hepatitis C treatment by 60% for civilians.
Important Outcomes and Lessons Learned
The outcome of Poghosyan v. Georgia, and subsequent actions, demonstrates the ways in which a series of cases brought before the ECtHR can help facilitate legislative change to create programs for Hepatitis C patients in prisons and effectively reduce price barriers of medicines for populations in low-income countries. Legislation can play a key role in raising the profile of the problem and securing political commitment, paired with a combination of other tactics, including advocacy campaigns.
In this case, Open Society Georgia Foundation, along with lawyers and civil society organizations, partnered to assume an active role in developing jurisprudence on increasing the efficacy of treatment for incarcerated individuals with Hepatitis C. In developing an effective strategy, these parties focused their efforts on attacking one of the biggest barriers toward treatment – the exorbitant price tag of HCV treatment. In the aftermath of Poghosyan v. Georgia, Georgia’s prevention and treatment program has been lauded the first example of its kind amongst low- and middle- income countries and a model that other countries should follow.
Governments might also consider the prevalence of Hepatitis C in prisons as an important public health opportunity.[204] If governments can effectively address the spread of Hepatitis C in prisons, the burden of disease in the population as a whole will drastically decrease. In fact, recent pharmaco-economic analyses suggest that treatment of Hepatitis C in prisons in the short term is a cost effective investment in the long term, reducing total HCV health expenditures.[205] “There’s a tsunami of death and disease that’s already starting to crash down on us, and will continue to in the decades ahead,” Josiah Rich observed, who has written a new analysis on the matter. “But now that treatment can dramatically reduce transmission of this virus, we’re getting closer and closer to ending this epidemic. We argue that we should use the correctional system to do that.”[206
5. Where can I find additional resources on access to medicines and human rights?
A list of commonly used resources on patient care and human rights follows. It is organized into the following categories:
- International Instruments
- Regional Instruments
- General Resources
- Patents and Human Rights
- The Concept of Essential Medicines
- Access to Medicines and the Role of the Courts
- Right to Life
- Right to Health
- Right to Enjoy the Benefits of Scientific Progress and its Applications
- Children
- Women
- Key Populations – Prisoners
- Key Populations – Patients with HIV/AIDS
- Key Populations – Patients with Cancer
- Key Populations – Patients with TB
- Key Populations – Older people
- Key Populations – Neglected diseases
- Websites
International Instruments
- Human Rights Council, Access to Medicines in the Context of the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health, A/HRC/23/L.10/Rev.1, June 11, 2013, https://documents-dds-ny.un.org/doc/UNDOC/LTD/G13/147/13/PDF/G1314713.pdf?OpenElement.
- Human Rights Council, Elaboration of an International Legally Binding Instrument on Transnational Corporations and other Business Enterprises with Respect to Human Rights, A/HRC/26/L.22, June 26, 2014, https://documents-dds-ny.un.org/doc/UNDOC/LTD/G14/058/99/PDF/G1405899.pdf?OpenElement.
- Office of the High Commissioner for Human Rights, Human Rights Guidelines for Pharmaceutical Companies in Relation to Access to Medicines in General Assembly of the UN Special Rapporteur on the Right to the Highest Attainable Standard of Health, A/63/263 (Aug. 11, 2008), http://www.ifhhro.org/images/stories/ifhhro/documents_UN_special_rapporteur/3_4_8.pdf.
- UN Commission on Human Rights, Access to Medication in the Context of Pandemics such as HIV/AIDS, Tuberculosis and Malaria, Resolutions 2005/23, 2004/26, 2003/29 & 2002/32, ohchr.org/EN/Issues/HIV/Pages/Documents.aspx.
- UN Commission on the Status of Women, Women, the Girl Child and HIV and AIDS, Resolution 55/2, E/CN.6/2011/L.3 (2011).
www.un.org/womenwatch/daw/csw/csw55/other-outcomes/HIVandAIDS-adv-unedit.pdf. - The Limburg Principles on the Implementation of the International Covenant on Economic, Social and Cultural Rights, U.N. Doc. E/CN.4/1987/17, Annex at para. 17 and 18, https://www.escr-net.org/docs/i/425445.
- UN Committee on Economic, Social and Cultural Rights, General Comment No. 14, U.N. Doc. E/C.12/2000/4 (Aug. 11, 2000).
- UN General Assembly, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Anand Grover, on access to medicines, A/HRC/23/42 (May 1, 2013).
- UN Doc. A/HRC 17/43: Report of the expert consultation on access to medicines as a fundamental component of the right to health.
- UN Committee on Economic, Social and Cultural Rights, Human Rights and Intellectual Property, 27th Sess., ¶ 12, U.N Doc. E/C.12/2001/15 (2001).
- UN Sub-Commission on Human Rights, Resolution 2000/7, Intellectual Property Rights and Human Rights, U.N. Doc. A/CN.4/L.682
- World Health Organization, Constitution of the World Health Organization (adopted in 1946), http://www.who.int/governance/eb/who_constitution_en.pdf.
- World Health Organization, Declaration of Alma-Ata (September 6-12, 1978), www.who.int/publications/almaata_declaration_en.pdf.
Regional Instruments
African Commission on Human and Peoples’ Rights, Resolution on Access to Health and Needed Medicines in Africa, ACHPR/Res.141 (XXXXIIIII) 08 (November 2008). achpr.org/sessions/44th/resolutions/141/.
- Council of Europe, Convention for the Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine (1997). http://conventions.coe.int/Treaty/EN/Treaties/Html/164.htm.
- European Union, Programme for Action to Confront HIV/AIDS, Malaria and Tuberculosis (2007-2011), COM(2005) 179. http://europa.eu/legislation_summaries/development/sectoral_development_policies/r12537_en.htm.
- World Health Organization, Scaling up response the response to HIV/AIDS in the European Region of WHO, Resolution EUR/RC52/R9 (2002). www.euro.who.int/Governance/resolutions/2002/20021231_4
- World Health Organization, The Berlin Declaration on Tuberculosis, European Ministerial Forum, EUR/07/5061622/5 (Oct. 22, 2007). euro.who.int/__data/assets/pdf_file/0008/68183/E90833.pdf.
General Resources
- Alicia Ely Yamin, “Not Just a Tragedy: Access to Medications as a Right under International Law,” Boston University International Law Journal 325 (2003).
- D. Quick and H. V. Hogerzeil, “Perspectives: Twenty-five Years of Essential Medicines,” Bulletin of the World Health Organization 80, 161-167.
- Joint United Nations Programme on HIV and AIDS (UNAIDS), “Access to Medicines: Challenges and Opportunities for Developing Countries,” UNAIDS website, May 20, 2014, http://www.unaids.org/en/resources/presscentre/featurestories/2014/may/20140520brics.
- Maryam Bigdeli, Bart Jacobs, Goran Tomson, et al., “Access to Medicines from a Health Systems Perspective,” Health Policy and Planning 28 (2013), 692-704.
- Office of the High Commissioner for Human Rights, “UN Independent Expert Launches Draft Human Rights Guidelines for Pharmaceutical Companies,” press release, September 19, 2007, http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=2550&LangID=E#sthash.myfJUVJF.dpuf.
- Paul Hunt and Rajat Khosla, “The Human Right to Medicines,” Sur: International Journal on Human Rights 8 (2008), file:///P:/HHRG/Materials/Human%20Rights%20to%20Medicine.htm, 99–114.
- World Health Organization, “Equitable Access to Essential Medicines: A Framework for Collective Action,” Policy Perspectives on Medicines 8 (2004).
- World Health Organization, WHO Medicines Strategy: Countries at the Core: 2004-2007 (Geneva: WHO, 2004), http://www.who.int/management/background_4a.pdf.
- World Health Organization, “Access to Medicines” fact sheet, http://www.who.int/trade/glossary/story002/en/.
Intellectual Property and Human Rights
- Charles T. Collins-Chase, “The Case against TRIPS-Plus Protection in Developing Countries Facing Aids Epidemics,” University of Pennsylvania Journal of International Law29/763 (2014), http://scholarship.law.upenn.edu/jil/vol29/iss3/6.
- Jennifer Sellin, Access to Medicines: The Interface Between Patents and Human Rights: Does One Size Fit All? (Cambridge: Intersentia, 2014).
- Joo-Young Lee, A Human Rights Framework for Intellectual Property, Innovation and Access to Medicines (Farnham, England: Ashgate Publishing Limited, 2015).
- Laurence R. Helfer and Graeme W. Austin, Human Rights and Intellectual Property: Mapping the Global Interface (Cambridge, UK: Cambridge University Press, 2011).
- Lisa Forman, “Trade Rules, Intellectual Property, and the Right to Health,” Ethics & International Affairs 21/3 (Fall 2007), 337—357, http://onlinelibrary.wiley.com/doi/10.1111/j.1747-7093.2007.000103.x/abstract.
- Médecins Sans Frontières, “The Impact of Patents on Access to Medicines,” http://www.msfaccess.org/content/impact-patents-access-medicines.
- Médecins Sans Frontières, “TRIPS, TRIPS Plus and Doha” (July 2011), http://www.msfaccess.org/content/trips-trips-plus-and-doha.
- Southern African Development Community (SADC), Statement of the Participants of the SADC Parliamentary Forum Training on Intellectual Property, Trade and Access to Medicines, May 14, 2009, Pretoria, South Africa,
- World Health Organization, Essential Medicines and Health Products Information Portal: A World Health Organization resource, Implications of the Doha Declaration on the Trips Agreement and Public Health – Health Economics and Drugs Series No. 012, http://apps.who.int/medicinedocs/en/d/Js2301e/9.html.
- World Trade Organization, Understanding the WTO: The Agreements, “Intellectual property: protection and enforcement,” https://www.wto.org/english/thewto_e/whatis_e/tif_e/agrm7_e.htm.
- World Trade Organization, Trips and Health: Frequently Asked Questions: Compulsory licensing of pharmaceuticals and TRIPS, https://www.wto.org/english/tratop_e/trips_e/public_health_faq_e.htm.
- Global Health Justice Partnership, A Human Rights Approach to Intellectual Property and Access to Medicines (New Haven, CT: Yale Law School and Yale School of Public Health, September 2013), http://apps.who.int/medicinedocs/en/d/Js20952en/.
The Concept of Essential Medicines
Hans V. Hogerzeil, “Essential Medicines and Human Rights: What Can They Learn From Each Other?” Bulletin of the World Health Organization 84 (2006), 371-375, http://www.who.int/bulletin/volumes/84/5/371.pdf.
- Ellen ‘t Hoen and Kaitlin Mara (with support from UNITAID), Ensuring that Essential Medicines are also Affordable Medicines: Challenges and Options (Geneva: World Health Organization, 2016), http://apps.who.int/medicinedocs/documents/s22345en/s22345en.pdf.
- Word Health Organization, “The Selection of Essential Medicines,” Policy Perspectives on Medicines 4 (2002).
- World Health Organization, “Essential Medicines,” http://www.who.int/topics/essential_medicines/en/.
Access to Medicines and the Role of the Courts
- Alicia Ely Yamin and Siri Gloppen (eds), Litigating Health Rights: Can Courts Bring More Justice to Health?(Cambridge, MA: Harvard University Press, 2011).
- Hans V. Hogerzeil, Melanie Samson, Jaume Vidal Casanovas, et al., “Is Access to Essential Medicines as Part of the Fulfilment of the Right to Health Enforceable Through the Courts?” Lancet 368 (2006), 305–11, http://www.who.int/medicines/news/Lancet_EssMedHumanRight.pdf.
- Ole Frithjof Norheim and Bruce M. Wilson, “Health Rights Litigation and Access to Medicines: Priority Classification of Successful Cases from Costa Rica’s Constitutional Chamber of the Supreme Court,” Health and Human Rights 16/2 (October 2014), http://www.hhrjournal.org/2014/10/02/health-rights-litigation-and-access-to-medicines-priority-classification-of-successful-cases-from-costa-ricas-constitutional-chamber-of-the-supreme-court/.
Access to Medicines and the Role of Pharmaceutical Companies
- Emmanuel Oke, “Using the Right to Health to Enforce the Corporate Responsibilities of Pharmaceutical Companies with Regard to Access to Medicines,” Journal of Health Diplomacy 1/1 (July 2013), http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2332604.
- Lisa Forman and Jillian Clare Kohler (eds), Access to Medicines as a Human Right: Implications for Pharmaceutical Industry Responsibility (Toronto: University of Toronto Press, 2012).
- Sofia Gruskin and Zyde Raad, “Are Drug Companies Living Up to Their Human Rights Responsibilities? Moving Toward Assessment,” PLoS Medicine 7/9 (September 2010), http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000310.
Right to Life
- De Vos et al, “Health through people’s empowerment: A rights-based approach to participation,” Health and Human Rights 11/1 (2009), www.hhrjournal.org/index.php/hhr/article/view/126/201.
- Alicia Ely Yamin, “Suffering and Powerlessness: The Significance of Promoting Participation in Rights-Based Approaches to Health,” Health and Human Rights 11/1 (2009), 5-22, hhrjournal.org/index.php/hhr/article/view/127/200.
Right to Health
- BMA and the Commonwealth Medical Trust, The Right to Health: A Toolkit for Health Professionals (June 2007), http://www.ifhhro.org/our-work/our-publications/353-the-right-to-health-a-toolkit-for-health-professionals-2007.
- Hans V. Hogerzeil and Zafar Mirza, “Access to Medicines as Part of the Right to Health,” in The World Medicines Situation 2011 (Geneva: WHO, 2011), http://apps.who.int/medicinedocs/documents/s18772en/s18772en.pdf.
- Office of the High Commissioner for Human Rights and World Health Organization, The Right to Health, Fact Sheet No. 31, http://www.ohchr.org/Documents/Publications/Factsheet31.pdf.
- Stephen P. Marks, “Access to Essential Medicines as a Component of the Right to Health” in Health: A Human Rights Perspective, https://www.hsph.harvard.edu/wp-content/uploads/sites/580/2012/10/marks_access_to_essential_medecines-2009.pdf.
- UN General Assembly, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Anand Grover, on access to medicines, A/HRC/23/42 (May 1, 2013).
Right to Enjoy the Benefits of Scientific Progress and its Applications
- UN Committee on Economic, Social and Cultural Rights, General Comment No. 17: The right of everyone to benefit from the protection of the moral and material interests resulting from any scientific, literary or artistic production of which he is the author (art. 15 (1) (c)), E/C.12/GC/17 (2006). http://tb.ohchr.org/default.aspx?Symbol=E/C.12/GC/17.
Children
- World Health Organization, Essential Medicines for Children: Background Information: Child-specific medicines: A global priority, http://www.who.int/childmedicines/media/backgrounder/BG1/en/.
Women
- Human Rights Watch, “Stop Making Excuses”: Accountability for Maternal Health Care in South Africa (HRW, August 2011), http://reliefweb.int/sites/reliefweb.int/files/resources/Full_Report_2004.pdf.
- World Health Organization, WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage (Geneva: WHO, 2012).
Key Populations – Prisoners
- Rick Lines, “The right to health of prisoners in international human rights law,” International Journal of Prisoner Health 4/1 (March 2008), 3-53, www.ahrn.net/library_upload/uploadfile/file3102.pdf
Key Populations – Patients with HIV/AIDS
- Brazilian International AIDS Association/ Global AIDS Policy Watch, “HIV and AIDS in the mandate of the Special Rapporteur on the Right to Health: genealogies, lessons learned, challenges that remain,” December 10, 2014, http://abiainternacional.fw2.com.br/news/articles/hiv-and-aids-genealogies-lessons-learnd-and-challenges/124.
- Human Rights Watch (HRW), “The FTAA, Access to HIV/AIDS Treatment, and Human Rights,” Briefing Paper, October 29, 2002, https://www.hrw.org/report/2002/10/29/ftaa-access-hiv/aids-treatment-and-human-rights/human-rights-watch-briefing-paper.
- Lisa Forman, “A Transformative Power? The Role of the Human Right to Medicines in Accessing AIDS Medicines – International Human Rights Law, TRIPS, and the South African Experience” (SJD dissertation, University of Toronto, 2007).
- World Health Organization, Bulletin of the World Health Organization, “Access to AIDS medicines stumbles on trade rules,” http://www.who.int/bulletin/volumes/84/5/news10506/en/.
Key Populations – Patients with Cancer
- Ellen ‘t Hoen, Access to Cancer Treatment: A Study of Medicine Pricing issues with Recommendations for Improving Access to Cancer Medication (Oxford: Oxfam International, 2015), http://apps.who.int/medicinedocs/documents/s21758en/s21758en.pdf.
Key Populations – Patients with TB
- Ann M. Ginsberg and Melvin Spigelman, “Challenges in Tuberculosis Drug Research and Development,” Nature Medicine 13/3 (March 2007), http://www.tballiance.org/newscenter/research_papers/NatMed13_290_GinsbergSpigelman_Challenges%20in%20tuberculosis%20drug%20research%20and%20development.pdf.
Key Populations – Older people
- International Narcotics Control Board, Report of the International Narcotics Control Board on the Availability of Internationally Controlled Drugs: Ensuring Adequate Access for Medical and Scientific Purposes (2010), http://www.unodc.org/documents/southerncone/noticias/2011/03-marco/Jife/Report_of_the_Board_on_the_availability_of_controlled_substances.pdf.
- International Association for Hospice and Palliative Care, IAHPC List of Essential Medicines for Palliative Care (2007), http://hospicecare.com/resources/palliative-care-essentials/iahpc-essential-medicines-for-palliative-care/.
- Manfred Nowak and Anand Grover, Joint letter by UN special rapporteur on the prevention of torture and cruel, inhuman or degrading treatment or punishment, Manfred Nowak, and the UN special rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Anand Grover, to the Commission on Narcotic Drugs (December 2008). http://www.hrw.org/news/2008/12/10/un-human-rights-experts-call-upon-cnd-support-harm-reduction.
- E.C. Gispen, “A Human Rights View on Access to Controlled Substances for Medical Purposes under the International Drug Control Framework,” European Journal of Pharmacology 16 (2013).
Neglected Diseases
- UNICEF, UNDP, World Bank, World Health Organisation Special Programme for Research and Training in Tropical Diseases.
- Mary Moran, Anne-Laure Ropars, Javier Guzman, et al., The New Landscape of Neglected Disease Drug Development (London: The Wellcome Trust, 2005), http://www.policycures.org/downloads/The_new_landscape_of_neglected_disease_drug_development.pdf.
Websites
- European Public Health Alliance: http://epha.org.
- Health Rights: Human Rights in Patient Care: health-rights.org/.
- Physicians for Human Rights: org/.
- accesstomedicines.org
6. What are the key terms related to access to medicines and human rights?
Antiretroviral (ARV) and Antiretroviral Treatment (ART):
A medicine for the treatment of HIV. There are several classes of ARVs, which all target a different phase in the reproductive cycle of the virus. ART is a treatment regimen composed of several ARVs (usually three).[207]
Bolar exemption
A legal exemption that permits the use of patented invention before the patent expires for the purposes of obtaining marketing approval of a generic for commercialization once the patent expired.[208]
Compulsory license/ government use:
A compulsory licence is an authorisation by a competent government authority to use a patented invention by a third party without the consent of the patent holder, against a payment of “adequate remuneration.” A ‘government use’ is a particular form of compulsory licence issued by the government for its own use or for the use of a third party.[209]
Counterfeit medicine
WHO defines counterfeit medicine as “[a] medicine which is deliberately and fraudulently mislabelled with respect to identity and/or source. Counterfeiting can apply to both branded and generic products and counterfeit products may include products with the correct ingredients or with the wrong ingredients, without active ingredients, with insufficient active ingredients or with fake packaging.”[210]
Data exclusivity
Data exclusivity is the prohibition of use of pharmaceutical test data submitted to a regulatory agency by an originator company for the purpose of registering a generic drug. Generic companies rely on this test data to demonstrate the safety and efficacy of their bioequivalent drug. Delayed use of the data will therefore delay the registration and marketing of generic medicines, regardless of the patent status of the product.[211]
Delinkage
A term used to describe a key characteristic of any financing model of innovation characterized by the uncoupling of R&D costs and consume prices for health technologies. Examples of delinkage models include grants, prizes, and advance market commitments, among others.[212]
Doha Declaration on TRIPS and Public Health
The fourth World Trade Organization (WTO) ministerial conference in 2001 in Doha, Qatar responded to the public health concerns fuelled by the HIV/AIDS crisis by adopting the Doha Declaration on the Trade-Related Aspects of Intellectual Property Rights Agreement (TRIPS) and Public Health. The Doha Declaration, as it is widely known, affirmed the sovereign right of governments to take measures to protect public health, including the use of compulsory licensing and parallel importation. It also allowed least developed countries (LDCs) not to grant or enforce pharmaceutical product patents until at least 2016.[213]
Essential medicines
Essential medicines are those that satisfy the priority health care needs of the population. They are selected with due regard to public health relevance, evidence on efficacy and safety, and comparative cost-effectiveness.
Essential medicines are intended to be available within the context of functioning health systems at all times in adequate amounts, in the appropriate dosage forms, with assured quality and adequate information, and at a price the individual and the community can afford.[214]
Essential Medicines List (EML)
The EML is a list maintained by the World Health Organization that contains the most important medicines that should be available and affordable to the communities and people that need them. The EML is a tool for governments and healthcare providers seeking to meet the health needs of their populations. The EML is updated periodically to detail the medicines a health system should seek to make available.[215]
Evergreening
The practice of seeking secondary patents with the aim to extend market exclusivity beyond the patent term of the basic patent.[216]
Health
Complete physical, mental, and social well-being, rather than merely the absence of disease or infirmity (World Health Organization).
Intellectual property (IP)
Intellectual property (IP) refers to the legal rights that result from intellectual activity in the industrial, scientific, literary and artistic fields. IP has two branches: Industrial property (e.g., inventions (patents), trademarks, industrial designs, geographical indications) and copyright (and related rights).[217]
Neglected diseases
Diseases for which there is a lack of sufficient medical innovations, resulting in inadequate, ineffective or non-existent means to prevent, diagnose, and treat them. The lack of sufficient medical innovation is often rooted in an absence of market incentives owing to the low purchasing power of the populations disproportionately affected by such conditions.[218]
Orphan disease
A disease that affects only small numbers of individuals. The threshold number varies from country to country. An orphans disease may affect fewer than 2000,000 individuals (United States), fewer than 50,000 (Japan), or less than 2,000 (Australia). Definitions vary from diseases affecting about 1 to 8 in 10,000 individuals.[219]
Parallel importation
Parallel importation refers to the import and resale in a country, without the consent of the patent holder, of a patented product that has been legitimately put on the market of the exporting country. Parallel imports take place when there are significant price differences for the same good in different markets.[220]
Patent
A patent is a form of IP granted to an inventor for the creation of something new, non-obvious to a person who is knowledgeable in the field, and useful. Patents grant a temporary monopoly (usually 20 years), during which time the patent holder can prevent others from making, using, or selling their invention. A patent is national in nature, and inventors must apply under each countries patent laws in order to receive protection in that country. In international trade, however, a blocking patent in either the country of import or export could interfere. That 148 ANNEXES means a patent in a country that produces lots of generic medicines, such as India, can be enough to restrict access to those medicines in other countries relying on the first country’s exports, regardless of whether or not there is a patent in the importing country.[221]
Patentability criteria
Requirements that must be satisfied before a patent is awarded. These are (1) subject matter for eligibility, (2) novelty, (3) an inventive step and (4) industrial application. The precise nature of these requirements is not defined in the TRIPS Agreement and it is up to countries to define these in their laws and policies.[222]
Patent pools
An agreement among patent holders to voluntarily license a set of their patents to one another or to third parties. Patent pools are often administered or managed by institutional frameworks to facilitate the negotiation of such agreements.[223]
Patient
A user of health care services, whether healthy or sick (Declaration on the Promotion of Patients’ Rights in Europe, WHO, Amsterdam 1994).
A person in contact with the health system, seeking attention for a health condition (European Observatory on Health Systems and Policies).
Stigma and discrimination
The United Nations has called stigma and discrimination associated with HIV and AIDS “the greatest barriers to preventing further infections, providing adequate care, support and treatment and alleviating impact.” Stigmatization leads to discrimination.
Stigma is “a powerful discrediting and tainting social label that radically changes the way individuals view themselves and are viewed as persons.” People who are stigmatized are usually considered deviant or shameful for some reason or other, and as a result are shunned, avoided, discredited, rejected, restrained or penalized. As such, stigma is an expression of social and cultural norms, shaping relationships among people according to those norms. Stigma marks the boundaries a society creates between “normals” and “outsiders,” between “us” and “them.”
Discrimination “refers to unfair or unjustifiably adverse treatment.”[224] Discrimination can be legitimate and illegitimate. Illegitimate discrimination is unjustified, disproportionate, and arbitrary. A measure or an action is unjustified if it lacks rational and objective reasons. It is disproportionate if the means employed and their consequences far exceed or do not achieve the aims pursued. It is arbitrary if it seriously infringes the rights of the individual and is not necessary to protect the health of others.
The Trade Related Aspects of Intellectual Property Rights Agreement (TRIPS)
Administered by the World Trade Organization, TRIPS sets out minimum standards for the protection of several forms of IP that all World Trade Organization member countries need to implement. TRIPS also contains several important flexibilities to preserve the rights of nations to protect the public interest.[225]
TRIPS flexibilities
A term used broadly to describe a set of norms, rules, and standards that allow variations in the implementation of the TRIPS Agreement obligations, including limits on the exercise of intellectual property rights.[226]
TRIPS-Plus/ TRIPS+
These are measures that require more stringent IP standards than those contained in TRIPS or that limit flexibilities inherent in TRIPS. They are often contained in bilateral or regional trade agreements, and are a matter of concern for public health advocates.[227]
Voluntary license
A license granted by a patent holder to a third party to produce and/or market and distribute a patented product, usually in exchange for a royalty on net sales and certain other conditions (for example, geographical restrictions on where the product can be sold).[228]
World Health Assembly (WHA)
Attended by health ministers from World Health Organization member states, the WHA is the most important World Health Organization (WHA) governing body, setting the direction and priorities for the organisation at its annual meeting. [229]
WHO
The Word Health Organization (WHO) is the directing and coordinating authority on international health within the United Nations’ system. The WHO does this by: providing leadership on matters critical to health and engaging in partnerships where joint action is needed; shaping the research agenda and stimulating the generation, translation and dissemination of valuable knowledge; setting norms and standards and promoting and monitoring their implementation; articulating ethical and evidence-based policy options; providing technical support, catalysing change, and building sustainable institutional capacity; and monitoring the health situation and assessing health trends.[230]
WIPO
The World Intellectual Property Organization (WIPO) is the global forum for intellectual property services, policy, information and cooperation. It is a self-funding agency of the United Nations, with 189 member states.[231]
WTO
The World Trade Organization (WTO) is the only global international organization dealing with the rules of trade between nations. At its heart are the WTO agreements, negotiated and signed by the bulk of the world’s trading nations and ratified in their parliaments. The goal is to ensure that trade flows as smoothly, predictably and freely as possible.[232]
[1] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 3.
[2] Ibid., 3.
[3] United Nations (UN), “Goal 3: Ensure healthy lives and promote well-being for all at all ages,” SDGs fact sheet, http://www.un.org/sustainabledevelopment/health/.
[4] Access to Medicine Foundation, “The 2016 Access to Medicine Index: Methodology 2015,” 2016, http://apps.who.int/medicinedocs/documents/s22176en/s22176en.pdf [accessed 27 April 2017].
[5] United Nations (UN), “Goal 3: Ensure healthy lives and promote well-being for all at all ages,” SDGs fact sheet, http://www.un.org/sustainabledevelopment/health/.
[6] While access to treatment for HIV/AIDS is still a challenge for many, “new HIV infections in 2013 were estimated at 2.1 million, which was 38 per cent lower than in 2001.” United Nations (UN), “Goal 3: Ensure healthy lives and promote well-being for all at all ages,” SDGs fact sheet, http://www.un.org/sustainabledevelopment/health/.
[7] In 2014 alone NTDs affected an estimated 1.7 billion people. However, insufficient R&D is invested in treating and preventing NTDs, “further amplified by the fact that many [of these diseases] require chronic and costly care.” WHO, World Health Statistics 2016: Monitoring Health for the Sustainable Development Goals (Geneva: WHO, 2016) in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 13.
[8] UN Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, U.N. Doc. E/C.12/2000/4 (August 11, 2000).
[9] Ibid, paragraph 43(d).
[10] UN General Assembly, The Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health: Report of the Special Rapporteur, Paul Hunt, U.N. General Assembly, 63rd Session, Agenda Item 67(b), U.N. Doc, A/63/263 (August 11, 2008).
[11] John Ruggie, Report of the Special Representative of the Secretary-General on the Issue of Human Rights
and Transnational Corporations and Other Business Enterprises: ‘Protect, Respect and Remedy: A
Framework for Business and Human Rights’, A/HRC/8/5 (April 7, 2008).
[12] Article 2(1) of the ICESCR calls upon all states, individually “and through international assistance and cooperation,” to guarantee the progressive realization of human rights.
[13] UN Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, para. 40.
[14] Xavier Seuba states that “WHO mentions the recognition of access to essential medicines as a human right at the state level among the priorities in the framework of implementation of pharmaceutical policies in the period 2004-2007, and WHO’s joint effort with the United Nations Committee on Economic, Social, and Cultural Rights has resulted in the inclusion of access to essential medicines in the core content of the right to health. See Xavier Seuba, “Round Table: A Human Rights Approach to the WHO Model List of Essential Medicines,” Bulletin of the World Health Organization 84 (2006), http://apps.who.int/medicinedocs/documents/s21845en/s21845en.pdf, 405-411.
[15] See UN Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, U.N. Doc. E/C.12/2000/4 (August 11, 2000).
[16] For a brief explanation of these principles, see UN Development Group (UNDG), The Human Rights Based Approach to Development Cooperation Towards a Common Understanding Among UN Agencies (May 2003), http://hrbaportal.org/the-human-rights-based-approach-to-development-cooperation-towards-a-common-understanding-among-un-agencies.
[17] UN Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, U.N. Doc. E/C.12/2000/4 (August 11, 2000).
[18] OHCHR/WHO, The Right to Health, Factsheet No. 31, 2008.
[19] Hans V. Hogerzeil, Melanie Samson, Jaume Vidal Casanovas, et al., “Is Access to Essential Medicines as Part of the Fulfilment of the Right to Health Enforceable through the Courts?” Lancet 368 (July 2006), pp. 305-11, http://cdrwww.who.int/medicines/news/Lancet_EssMedHumanRight.pdf.
[20] I. Khan and D. Petrasek, “Beyond the Courts – Protecting Economic and Social Rights,” OpenDemocracy, 2014, https://www.opendemocracy.net/openglobalrights/irene-khan-david-petrasek/beyond-courts-%E2%80%93-protecting-economic-and-social-rights [Accessed April 27, 2017].
[21] ICESCR Committee General Comment No. 14.
[22] See CESCR General Comment No. 14: “If resource constraints render it impossible for a State to comply fully with its Covenant obligations, it has the burden of justifying that every effort has nevertheless been made to use all available resources at its disposal in order to satisfy … the obligations outlined above.”
[23] See the public health flexibilities available under TRIPS, for example, compulsory licensing, parallel importation, and discretion in defining domestic standards of patentability.
[24] States have a duty to protect human rights, corporations have a duty to respect human rights, and states must ensure that there is access to effective remedy when abuses occur within their territory and/or jurisdiction.
[25] John Ruggie, Report of the Special Representative of the Secretary-General on the Issue of Human Rights
and Transnational Corporations and Other Business Enterprises: ‘Protect, Respect and Remedy: A
Framework for Business and Human Rights’, A/HRC/8/5 (April 7, 2008). For additional normative statements on the human rights responsibilities of corporations, see: the UN Sub-Commission on the Promotion and Protection of Human Rights; the UN Global Compact, and the Organization for Economic Cooperation and Development (OECD) Guidelines for Multinational Enterprises.
[26] UN Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, U.N. Doc. E/C.12/2000/4 (August 11, 2000).
[27] WHO, “Equitable Access to Essential Medicines: A Framework for Collective Action” in WHO Policy Perspectives on Medicines Bulletin(2004), http://apps.who.int/medicinedocs/pdf/s4962e/s4962e.pdf, 2.
[28] See the Limburg Principles, https://www.escr-net.org/docs/i/425445.
[29] See Additional Protocol to the American Convention on Human Rights in the Area of Economic, Social And Cultural Rights “Protocol of San Salvador,” http://www.oas.org/juridico/english/treaties/a-52.html.
[30] WHO, Constitution of the World Health Organization, http://www.who.int/gb/bd/PDF/bd46/ebd46_p2.pdf.
[31] WHO, Declaration of Alma-Ata, International Conference on primary health care, Alma-Ata, USSR, 6–12 September, 1978, http://www.searo.who.int/LinkFiles/Health_Systems_declaration_ almaata.pdf.
[32] WHO, The Bangkok Charter for Health Promotion in a Globalized World, 2005 http://www.who.int/healthpromotion/conferences/ 6gchp/hpr_050829_%20BCHP.pdf.
[33] Gunilla Backman, Paul Hunt, Rajat Khosla, et al., “Health Systems and the Right to Health: An Assessment of
194 Countries,” Lancet 372 (2008), 2047–85, http://www.who.int/medicines/areas/human_rights/Health_System_HR_194_countries.pdf.
[34] WHO, Declaration of Alma-Ata, International Conference on Primary Health Care, Alma-Ata, USSR, September 6-12, 1978 http://www.searo.who.int/LinkFiles/Health_Systems_declaration_almaata.pdf (accessed Sept 21, 2008).
[35] Jody Heymann, Adèle Cassola, Amy Raub, et al., “Constitutional Rights to Health, Public Health and Medical Care: The Status of Health Protections in 191 Countries,” Global Public Health 8/6 (2013), pp. 639-653, http://www.tandfonline.com/doi/abs/10.1080/17441692.2013.810765.
[36] S. Katrina Perehudoff, Brigit Toebes, and Hans Hogerzeil, “Essential Medicines in National Constitutions: Progress Since 2008,” Health and Human Rights 18/1 (June 2016), pp. 141–156, https://www.hhrjournal.org/2016/05/essential-medicines-in-national-constitutions-progress-since-2008/.
[37] Paul Hunt and Rajat Khosla, “Are Drug Companies Living Up to Their Human Rights Responsibilities? The Perspective of the Former United Nations Special Rapporteur (2002-2008),” PLoS Medicine 7/9 (2010), http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000330.
[38] Ibid.
[39] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 16.
[40] See TRIPS Article 27: “[P]atents shall be available for any inventions, whether products or processes, in all fields of technology, provided that they are new, involve an inventive step and are capable of industrial application.”
[41] Ellen ’t Hoen, Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), pg. 90.
[42] Commission on Intellectual Property Rights, Integrating Intellectual Property Rights and Development Policy: Report of the CIPR (London: UK Commission on Intellectual Property Rights, 2002), 21, quoted in Jennifer Sellin, Access to Medicines: The Interface Between Patents and Human Rights: Does One Size Fit All?, 81.
[43] See also UN Sub-Commission on Human Rights, Resolution 2000/7, Intellectual Property Rights and Human Rights, U.N. Doc. A/CN.4/L.682.
[44] Global Commission on HIV and the Law, Risks, Rights and Health (New York: UNDP, July 2012), http://www.hivlawcommission.org/resources/report/FinalReport-Risks,Rights&Health-EN.pdf.
[45] Médecins Sans Frontières (MSF), “The Impact of Patents on Access to Medicines,” MSF website, http://www.msfaccess.org/content/impact-patents-access-medicines.
[46] The European Consumer Organisation, Position on Access to Medicines (Brussels: BEUC, 2015), http://www.beuc.eu/publications/beuc-x-2015-104_access_to_medicines.pdf.
[47] Ibid.
[48] UN General Assembly, Report of the Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health – Expert Consultation on Access to Medicines as a Fundamental Component of the Right to Health, UN Doc. A/HRC 17/43 (March 16, 2011).
[49] Paul Farmer, Pathologies of Power: Health, Human Rights, and the New War on the Poor (Berkeley and Los Angeles: University of California Press, 2013), 317.
[50] The Commission on Intellectual Property Rights, Innovation and Public Health, Public Health, Innovation and Intellectual Property Rights (Geneva: WHO, 2006), http://www.who.int/intellectualproperty/documents/thereport/ENPublicHealthReport.pdf?ua=1, 22.
[51] Ibid.
[52] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 8.
[53] Ibid.
[54] Lisa Forman, “A Transformative Power? The Role of the Human Right to Medicines in Accessing AIDS Medicines – International Human Rights Law, TRIPS, and the South African Experience” (SJD dissertation, University of Toronto, 2007).
[55] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), 22.
[56] World Trade Organization, “Intellectual Property: Protection and Enforcement” in Understanding the WTO: The Agreements, WTO fact sheet, https://www.wto.org/english/thewto_e/whatis_e/tif_e/agrm7_e.htm.
[57] “Some governments, such as Brazil, Thailand or India, have done precisely that.” Médecins Sans Frontières (MSF), “TRIPS, TRIPS Plus and Doha,” July 2011, http://www.msfaccess.org/content/trips-trips-plus-and-doha.
[58] United States Trade Representative (USTR), The Doha Declaration On The Trips Agreement And
Public Health, undated, https://ustr.gov/archive/assets/Trade_Sectors/Intellectual_Property/Public_Health/asset_upload_file511_4113.pdf.
[59] Ibid.
[60] World Trade Organization (WTO), Declaration on the TRIPS Agreement and Public Health, WT/MIN(01)/DEC/2 (November 20, 2001), https://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm.
[61] C. Li and K. Maskus, “The Impact of Parallel Imports on Investments in Cost-Reducing Research and Development,” Journal of International Economics 68 (2006), 443-455.
[62] K. Maskus, Parallel Imports in Pharmaceuticals: Implications for Competition and Prices in Developing Countries, Final Report to World Intellectual Property Organization (2001), http://www.wipo.int/export/sites/www/about ip/en/studies/pdf/ssa_maskus_pi.pdf [accessed January 24, 2017].
[63] C. Li and K. Maskus, “The Impact of Parallel Imports on Investments in Cost-Reducing Research and Development,” Journal of International Economics 68 (2006), 443-455.
[64] World Trade Organization (WTO), Declaration on the TRIPS Agreement and Public Health, WT/MIN(01)/DEC/2 (November 20, 2001), para 5(d).
[65] WTO, Extension of the Transition Period Under Article 66.1 of the TRIPS Agreement for Least Developed Country Members for Certain Obligations With Respect to Pharmaceutical Products, Decision of the Council for TRIPS of 6 November 2015 (2015), Doc No. IP/C/73.
[66] Ibid.
[67] Marceau, “WTO Dispute Settlement and Human Rights,” 755, in Jennifer Sellin, Access to Medicines.
[68] Joo-Young Lee, A Human Rights Framework for Intellectual Property, Innovation and Access to Medicines (Farnham, England: Ashgate Publishing Limited, 2015).
[69] Recommendation 2.6.1(a) from the High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016).
[70] UNITAID, Area for Intervention Related to Intellectual Property: Supporting the Use of TRIPS Flexibilities (Geneva: UNITAID, December 13-14, 2016), http://www.unitaid.eu/images/Resolutions/eb26/UNITAID_EB26_2016_R5_IP%20AfI.pdf.
[71] Charles T. Collins-Chase, “The Case against TRIPS-Plus Protection in Developing Countries Facing Aids Epidemics,” University of Pennsylvania Journal of International Law 29/763 (2014), http://scholarship.law.upenn.edu/jil/vol29/iss3/6.
[72] See Box 8 of the Final Report of the High-Level Panel for a comprehensive summary of all the TRIPS-plus provisions found in existing free trade agreements. See High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016).
[73] Ibid.
[74] WHO, Essential Medicines and Health Products Information Portal: A World Health Organization resource, Implications of the Doha Declaration on the Trips Agreement and Public Health – Health Economics and Drugs Series No. 012, http://apps.who.int/medicinedocs/en/d/Js2301e/9.html.
[75] Report of the Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health (2009), Human Rights Council, Eleventh Session, March 31, 2009, UN Document No. A/HRC/11/12, https://documents-dds-ny.un.org/doc/UNDOC/GEN/G09/127/11/PDF/G0912711.pdf?OpenElement [accessed April 27, 2017].
[76] Ibid.
[77] Recommendation 2.6.1(e) of the Final Report of the High-Level Panel on Access to Medicines.
[78] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 29.
[79] C. Clift et al., Towards a New Global Business Model for Antibiotics: Delinking Revenues from Sales. Report from Chatham House Working Group on New Antibiotic Business Models (2015), Chatham House, https://www.chathamhouse.org/sites/files/chathamhouse/field/field_document/20151009NewBusinessModelAntibioticsCliftGopinathanMorelOuttersonRottingenSo.pdf [accessed April 26, 2017].
[80] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 29.
[81] C. Clift et al., Towards a New Global Business Model for Antibiotics: Delinking Revenues from Sales. Report from Chatham House Working Group on New Antibiotic Business Models (2015), Chatham House, https://www.chathamhouse.org/sites/files/chathamhouse/field/field_document/20151009NewBusinessModelAntibioticsCliftGopinathanMorelOuttersonRottingenSo.pdf [Accessed 26 April 2017].
[82] WHO, Accelerating Work to Overcome the Global Impact of Neglected Tropical Diseases: A Roadmap for Implementation (Geneva: WHO, 2012),
http://www.who.int/neglected_diseases/NTD_RoadMap_2012_Fullversion.pdf
[83] Office of the High Commissioner for Human Rights (OHCHR), Human Rights Guidelines for Pharmaceutical Companies in Relation to Access to Medicines in General Assembly of the UN Special Rapporteur on the Right to the Highest Attainable Standard of Health, A/63/263 (August 11, 2008), http://www.ifhhro.org/images/stories/ifhhro/documents_UN_special_rapporteur/3_4_8.pdf.
[84] Ellen ‘t Hoen, Access to Cancer Treatment: A Study of Medicine Pricing issues with Recommendations for Improving Access to Cancer Medication (Oxford: Oxfam International, 2015), http://apps.who.int/medicinedocs/documents/s21758en/s21758en.pdf.
[85] Bloomberg News, “Roche Herceptin Copy’s Price Still Out of Reach in India,” January 20, 2014, http://www.bloomberg.com/news/articles/2014-01-20/roche-herceptin-copy-s-price-still-out-of-reach-in-india.
[86] The Telegraph, “Breast Cancer Sufferers Denied Two Drugs on NHS,” February 14, 2012, http://www.telegraph.co.uk/news/health/news/9079213/Breast-cancer-sufferers-denied-two-drugs-on-NHS.html.
[87] Paul Farmer, Pathologies of Power: Health, Human Rights, and the New War on the Poor (see note 49).
[88] Knowledge Ecology International, Transcript of Bayer CEO Marjin Dekkers, quote at the December 3, 2013 FT Event, regarding India compulsory license of Nexavar, http://keionline.org/node/1924.
[89] A disability adjusted life year can be thought of as one lost year of healthy life. See Ellen ‘t Hoen, Access to Cancer Treatment: A Study of Medicine Pricing issues with Recommendations for Improving Access to Cancer Medication (Oxfam, May 2014), http://apps.who.int/medicinedocs/documents/s21758en/s21758en.pdf.
[90] Paul Farmer, Pathologies of Power: Health, Human Rights, and the New War on the Poor (see note 49), 305.
[91] United Nations Secretary-General’s High-Level Panel on Access to Medicines, “The Process” (website), http://www.unsgaccessmeds.org/the-process/.
[92] Ellen ‘t Hoen, Brigit Toebes, Katrina Perehudoff, and Frederick Abbott, Submission to the UN High Level Panel on Access to Medicines by the Global Health Law Committee of the International Law Association, February 22, 2016, http://www.unsgaccessmeds.org/inbox/2016/2/22/contributionglobal-health-law-committee-of-the-international-law-association.
[93] James Love and Judit Rius, Submission to the UN High Level Panel on Access to Medicines by Knowledge Ecology International, February 29, 2016, http://www.unsgaccessmeds.org/inbox/2016/2/29/james-love.
[94] Els Torreele, Submission to the UN High Level Panel on Access to Medicines by Open Society Foundation, February 28, 2016, http://www.unsgaccessmeds.org/inbox/2016/2/28/els-torreele.
[95] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016).
[96] OHCHR and World Health Organization, The Right to Health, Fact Sheet No. 31, http://www.ohchr.org/Documents/Publications/Factsheet31.pdf.
[97] Ibid.
[98] Ibid.
[99] Alicia Ely Yamin, “Not Just a Tragedy: Access to Medications as a Right under International Law,” Boston University International Law Journal 21/2, 325-371, http://www.bu.edu/law/journals-archive/international/volume21n2/325-372.pdf.pdf.
[100] See, e.g., Human Rights and Intellectual Property, U.N. Comm. on Econ., Soc. & Cultural Rts., 27th Sess., ¶ 12, U.N Doc. E/C.12/2001/15 (2001).
[101] Paul Hunt and Rajat Khosla, “The Human Right to Medicines,” Sur: International Journal on Human Rights 8 (2008), 99-114.
[102] Ibid.
[103] OHCHR and World Health Organization, The Right to Health, Fact Sheet No. 31, http://www.ohchr.org/Documents/Publications/Factsheet31.pdf.
[104] World Health Organization, Bulletin of the World Health Organization, “Access to AIDS Medicines Stumbles on Trade Rules,” http://www.who.int/bulletin/volumes/84/5/news10506/en/.
[105] UN General Assembly, Political Declaration on HIV/AIDS: Intensifying our Efforts to Eliminate HIV/AIDS, A/RES/65/277 (June 10, 2011), www.unaids.org/en/media/unaids/contentassets/documents/document/2011/06/20110610_UN_A-RES-65-277_en.pdf.
[106] WHO, HIV/AIDS Fact Sheet (updated November 2015), http://www.who.int/mediacentre/factsheets/fs360/en/.
[107] UNAIDS, Global AIDS Epidemic Facts and Figures (July 18, 2012), www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/201207_FactSheet_Global_en.pdf.
[108] UNAIDS, Report on the Global AIDS Epidemic 2012 (2012), www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_with_annexes_en.pdf, 8-12.
[109] Ibid.
[110] WHO, “HIV/AIDS: Antiretroviral Therapy,” www.who.int/hiv/topics/treatment/en/.
[111] Ibid.
[112] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016).
[113] T. Fulda and P. Dickens, “Controlling the Cost of Drugs: The Canadian Experience,” Health Care Financing Review 1/2 (1979), 55-64.
[114] J. Reichman, “Compulsory Licensing of Patented Pharmaceutical Inventions: Evaluating the Options,” Journal of Law and Medical Ethics 37/2 (2009), 247–263.
[115] Ibid.
[116] Health24, “Red flag over HIV Medicine Stockout,” Health24, October 28, 2015, http://www.health24.com/Medical/HIV-AIDS/Living-with-HIV/Red-flag-over-HIV-medicine-stock-out-20151027 [accessed January 29, 2017].
[117] Fix The Patent Laws! “A Timeline of Intellectual Property Reform in South Africa: 1994-2016,” http://www.fixthepatentlaws.org/wp-content/uploads/2016/09/IP-reform-timeline-for-email.pdf [accessed January 9, 2017].
[118] Health24, “Red flag over HIV Medicine Stockout,” Health24, October 28, 2015, http://www.health24.com/Medical/HIV-AIDS/Living-with-HIV/Red-flag-over-HIV-medicine-stock-out-20151027 [accessed January 29, 2017].
[119] Ibid.
[120] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016).
[121] WHO, “Make Medicines Child Size,” http://www.who.int/childmedicines/en/.
[122] WHO, “Childhood Tuberculosis,” www.who.int/tb/challenges/children/en/index.html.
[123] WHO, “Make Medicines Child Size” (see note 121).
[124] Ibid.
[125] Ibid.
[126] Ibid.
[127] Ibid.
[128] World Health Organization, WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage (Geneva: WHO, 2012).
[129] Committee on Economic, Social and Cultural Rights, General Comment No. 22, The Right to Sexual and
Reproductive Health (article 12 of the International Covenant on Economic, Social and Cultural Rights), UN Doc. No. E/C.12/GC/22 (2016).
[130] Committee on the Elimination of Discrimination against Women, General Recommendation 24, Women and Health (Twentieth session, 1999), U.N. Doc. A/54/38 at 5 (1999), reprinted in Compilation of General Comments and General Recommendations Adopted by Human Rights Treaty Bodies, U.N. Doc. HRI/GEN/1/Rev.6 at 271 (2003), https://www1.umn.edu/humanrts/gencomm/generl24.htm.
[131] Human Rights Watch, “Stop Making Excuses”: Accountability for Maternal Health Care in South Africa (HRW, August 2011), http://reliefweb.int/sites/reliefweb.int/files/resources/Full_Report_2004.pdf.
[132] Ibid.
[133] OHCHR, “Upholding Women’s Human Rights Essential to Zika Response,” press release, February 5, 2016, http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=17014#sthash.6qsPD6Me.dpuf> [accessed April 27, 2017.
[134] For a complete discussion on harm reduction and freedom from torture and cruel, inhuman, and degrading treatment, including in prisons, see chapter 4 of this Resource Guide. Harvard FXB Center for Health and Human Rights/ Open Society Foundations, Harm Reduction and Human Rights (Boston: Harvard FXB/ OSF, 2013), https://www.hhrguide.org/2014/03/12/how-is-harm-reduction-a-human-rights-issue/.
[135] For the copy of the legal documents, news reports, and blog posts on the case, please see American Civil Liberties Union, Henderson et al. v. Thomas et al., www.aclu.org/hiv-aids-prisoners-rights/henderson-et-al-v-thomas-et-al.
[136] Ibid.
[137] Peter Loftus, “Prisoners Sue Massachusetts for Withholding Hepatitis C Drugs” New York Times, June 11, 2015, http://blogs.wsj.com/pharmalot/2015/06/11/prisoners-sue-massachusetts-for-withholding-hepatitis-c-drugs/.
[138] Alexandra Cameron, M. Ewen, Dennis Ross-Degnan et al., “Medicine Prices, Availability, and Affordability in 36 Developing and Middle-Income Countries: A Secondary Analysis,” Lancet 373 (2009), 240–49, http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)61762-6/abstract.
[139] Hans V. Hogerzeil, Jonathan Liberman, Veronika J. Wirtz et al., “Promotion of Access to Essential Medicines for Non-Communicable Diseases: Practical Implications of the UN Political Declaration,” Lancet 381 (2013), 680-9,
[140] M.E.C. Gispen, “A Human Rights View on Access to Controlled Substances for Medical Purposes under the International Drug Control Framework,” European Journal of Pharmacology 16 (2013).
[141] International Association for Hospice and Palliative Care, IAHPC List of Essential Medicines for Palliative Care (2007). http://hospicecare.com/resources/palliative-care-essentials/iahpc-essential-medicines-for-palliative-care/.
[142] Pallum India, “The Morphine Manifesto” (2012), http://palliumindia.org/manifesto/
[143] OHCHR and World Health Organization, The Right to Health, Fact Sheet No. 31, http://www.ohchr.org/Documents/Publications/Factsheet31.pdf.
[144] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 5.
[145] General comment No. 14, para. 18
[146] Ibid.
[147] Ibid.
[148] Ibid.
[149] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 9.
[150] Brazilian International AIDS Association/ Global AIDS Policy Watch, “HIV and AIDS in the Mandate of the Special Rapporteur on the Right to Health: Genealogies, Lessons Learned, Challenges that Remain,” December 10, 2014, http://abiainternacional.fw2.com.br/news/articles/hiv-and-aids-genealogies-lessons-learnd-and-challenges/124.
[151] Sigrun Skogly, Beyond National Borders: States’ Human Rights Obligations in International Cooperation (Antwerp, Netherlands: Intersentia, 2006), 13, 30; W. Vandenhole, “EU Obligations for Development: Extraterritorial Obligations under the ICESCR,” in M. Salomon, A. Tostensen, and W. Vandenhole (eds), Casting the Net Wider: Human Rights, Development and New Duty-Bearers (Antwerp, Netherlands: Intersentia, 2007); W. Vandenhole, “Is There a Legal Obligation to Cooperate Internationally for Development?” Convention of the Rights of the Child (CRC) — Report to General Day of Discussion (July 27, 2007), http://www.crin.org/docs/Vandenhole%20International%20Cooperation.pdf, p. 1.
[152] Committee on Economic, Social and Cultural Rights (see note 8), para. 40.
[153] Skogly et al. (see note 151).
[154] Sarah L. M. Davis, “Human Rights and the Global Fund to Fight AIDS, Tuberculosis, and Malaria,” Health and Human Rights 16/1 (July 2014), http://www.hhrjournal.org/2014/07/01/human-rights-and-the-global-fund-to-fight-aids-tuberculosis-and-malaria/.
[155] Joo-Young Lee, A Human Rights Framework for Intellectual Property, Innovation and Access to Medicines (Farnham, England: Ashgate Publishing Limited, 2015).
[156] InterAction, “HIV/AIDS, PEPFAR, and the Global Fund,” https://www.interaction.org/choose-to-invest-2017/hivaids-pepfar-global-fund.
[157] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 5.
[158] World Health Organization (WHO), World Intellectual Property Organization (WIPO) and World Trade Organization (WTO), Promoting Access to Medical Technologies and Innovation: Intersections between Public Health, Intellectual Property and Trade (Geneva: WHO, 2012), https://www.wto.org/english/res_e/booksp_e/pamtiwhowipowtoweb13_e.pdf in Ellen ’t Hoen, Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), 22.
[159] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 36.
[160] Ellen ’t Hoen, Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), 131.
[161] Ibid., 132.
[162] High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), 36.
[163] OHCHR, Human Rights Guidelines for Pharmaceutical Companies in Relation to Access to Medicines, http://www.ifhhro.org/images/stories/ifhhro/documents_UN_special_rapporteur/3_4_8.pdf.
[164] Ibid.
[165] Office of the United Nations High Commissioner for Human Rights, General Assembly of the UN Special Rapporteur on the right to the highest attainable standard of health (UN document: A/63/263, dated 11 August 2008), para. 45.
[166] hepCoalition.org, “Gilead’s License on Hepatitis C drugs, Sofosbuvir and Ledipasvir: A Fool’s Bargain: Myths and Facts,” http://www.hepcoalition.org/advocate/advocacy-tools/article/gilead-s-license-on-hepatitis-c.
[167] Office of the United Nations High Commissioner for Human Rights, General Assembly of the UN Special Rapporteur on the Right to the Highest Attainable Standard of Health.
[168] WHO, Medicines Policy, http://www.who.int/medicines/areas/policy/en/.
[169] Ole Frithjof Norheim and Bruce M. Wilson, “Health Rights Litigation and Access to Medicines: Priority Classification of Successful Cases from Costa Rica’s Constitutional Chamber of the Supreme Court,” Health and Human Rights 16/2 (October 2014), http://www.hhrjournal.org/2014/10/02/health-rights-litigation-and-access-to-medicines-priority-classification-of-successful-cases-from-costa-ricas-constitutional-chamber-of-the-supreme-court/.
[170] The majority of these cases were documented in Central and Latin America. Hans V. Hogerzeil, Melanie Samson, Jaume Vidal Casanovas, et al., “Is Access to Essential Medicines as Part of the Fulfilment of the Right to Health Enforceable Through the Courts?” Lancet 368 (2006), 305–11, http://www.who.int/medicines/news/Lancet_EssMedHumanRight.pdf.
[171] Stephen P. Marks, “Access to Essential Medicines as a Component of the Right to Health” in Health: A Human Rights Perspective, https://www.hsph.harvard.edu/wp-content/uploads/sites/580/2012/10/marks_access_to_essential_medecines-2009.pdf.
[172] Hans V. Hogerzeil, “Is Access to Essential Medicines as Part of the Fulfilment of the Right to Health Enforceable Through the Courts?”
[173] See generally, A. Yamin and S. Gloppen (eds), Litigating Health Rights: Can Courts Bring More Justice to Health? (Cambridge, MA: Harvard University Press, 2011).
[174] A. Yamin, “Will We Take Suffering Seriously? Reflections on What Applying a Human Rights Framework to Health Means and Why We Should Care,” Health and Human Rights 10/1 (2008).
[175] For a brief explanation of these principles, see UN Development Group (UNDG), The Human Rights Based Approach to Development Cooperation towards a Common Understanding among UN Agencies (May 2003), www.undg.org/archive_docs/6959-The_Human_Rights_Based_Approach_to_Development_Cooperation_Towards_a_Common_Understanding_among_UN.pdf.
[176] Ibid.
[177] Ibid.
[178] V. Gauri and S. Gloppen, Human Rights Based Approaches to Development: Concepts, Evidence, and Policy, World Bank Policy Research Working Paper 5938 (January 2012), http://elibrary.worldbank.org/content/workingpaper/10.1596/1813-9450-5938.
[179] The AIDS Law Project (ALP) is a non-governmental organization which works exclusively to promote equal rights and justice for people living with HIV and AIDS. See http://www.aidslawproject.org/about-aids-law-project/; see also http://www.ohchr.org/EN/Issues/Health/Pages/SRRightHealthIndex.aspx, and http://www.ohchr.org/EN/Issues/Health/Pages/SRBio.aspx.
[180] KELIN, Threat Posed by 2008 Anti-Counterfeit Act to Access Generic Medicines in Kenya (Kenya: KELIN, 2012), http://kelinkenya.org/wp-content/uploads/2010/10/Anti-Counterfeit-Act-to-Access-Generic-Medicines-in-Kenya-booklet.pdf.
[181] Anti-Counterfeit Act, 2008 CAP. 130A (An Act of Parliament to prohibit trade in counterfeit goods, to establish the Anti-Counterfeit Agency, and for connected purposes).
[182] Judgment: Petition No 409 of 2009, http://kelinkenya.org/wp-content/uploads/2010/10/Judgment-Petition-No-409-of-2009-Anti-counterfeit-case.pdf.
[183] Ibid.
[184] Ibid.
[185] Ibid.
[186] I-MAK, “India Rejects Sham Patent Application for Lifesaving HIV Drug: Pharmaceuticals in India now free to help HIV patients worldwide,” press release, January 2, 2011, http://static1.1.sqspcdn.com/static/f/129694/10047500/1294018171907/FINAL+Press+Release+1-1-2011.pdf?token=tGpdNo180J3KnXbdB33jTdjtoxg%3D
[187] The treatment combination is recommended by the World Health Organization, the Clinton Foundation HIV/AIDS Initiative, Medecins Sans Frontieres, and The Global Fund to Fight AIDS, Tuberculosis and Malaria and UNITAID.
[188] Tahir Amin and Aaron S. Kesselheim, “Secondary Patenting of Branded Pharmaceuticals: A Case Study of How Patents on Two HIV Drugs Could Be Extended for Decades,” Health Affairs 31/10 (2012), 2286-2294.
[189] I-MAK, “Patents and HIV Medications: An Overview,” fact sheet, http://static1.1.sqspcdn.com/static/f/129694/10047507/1294018196787/IMAK_FINALOverview+1-1-2011.pdf?token=yHodBvRmzldPdqWa%2BklwSrkRhmA%3D
[190] I-MAK, Pre-Grant Opposition, http://static1.1.sqspcdn.com/static/f/129694/996699/1294009496187/I-MAK+Pregrant+Opp+339+MUM+2006+.pdf?token=vjw3RSJ6CqDgkEQ54f68BlipssQ%3D.
[191] Médecins Sans Frontières, “Brazilians Demand Greater Access to Crucial HIV Drug,” November 10, 2011, https://msfaccess.org/resources/press-releases/1682.
[192] I-MAK, “India Rejects Sham Patent Application for Lifesaving HIV Drug: Pharmaceuticals in India now free to help HIV patients worldwide,” http://static1.1.sqspcdn.com/static/f/129694/10047500/1294018171907/FINAL+Press+Release+1-1-2011.pdf?token=tGpdNo180J3KnXbdB33jTdjtoxg%3D
[193] Ben Kiromba Twinomugisha, “Implications of the TRIPS Agreement for the Protection of the Right of Access to Medicines in Uganda,” Malawi Law Journal (2008), 253-278.
[194] Ibid.
[195] Reuters, “Gilead Uses Georgia as Free-Drug Testbed for Hepatitis C Elimination,” April 22, 2015, http://www.reuters.com/article/2015/04/22/us-health-hepatitis-gilead-georgia-idUSKBN0ND1XU20150422
[196] N. Chkhartishvili, L. Sharvadze, and O. Chokoshvili et al., “Mortality and Causes of Death among HIV-infected Individuals in the Country of Georgia,” AIDS Research and Human Retroviruses 30/6 (June 1, 2014), 1989–2012.
[197] E. Shapatava, K. E. Nelson, T. Tsertsvadze, and C. del Rio, “Risk Behaviors and HIV, Hepatitis B, and Hepatitis C Seroprevalence among Injection Drug Users in Georgia,” Drug and Alcohol Dependence 82/1 (2006), S35–8.
[198] (Georgia’s Ministry of Labor, Health, and Social Affairs [MoLHSA], unpublished data, 2015), Center for Disease Control (CDC), “Launch of a Nationwide Hepatitis C Elimination Program — Georgia, April 2015,” http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6428a2.htm.
[199] Azzi Momenghalibaf, “Georgia: A Leader in the Global Fight Against Hepatitis C,” Open Society Foundations blog, July 10, 2013, https://www.opensocietyfoundations.org/voices/georgia-leader-global-fight-against-hepatitis-c.
[200] Ibid.
[201] Ibid.
[202] European Court of Human Rights, “Structural inadequacy of medical care in prisons, in particular as regards the treatment of Hepatitis C: indication of appropriate legislative and other measures (Poghosyan v. Georgia)” in Information Note on the Court’s Case-Law, No. 116 (February 2009), http://www.echr.coe.int/Documents/CLIN_2009_02_116_ENG_851318.pdf.
[203] Ibid.
[204] Josiah D. Rich, Scott A. Allen, and Brie A. Williams, “Responding to Hepatitis C through the Criminal Justice System,” New England Journal of Medicine 370, 1871-1874, http://www.nejm.org/doi/full/10.1056/NEJMp1311941.
[205] See Mina Marmor and Henry I. Miller, “A Public Health And Healthcare Spending Time Bomb: Hepatitis C” (June 19, 2013), http://www.forbes.com/sites/henrymiller/2013/06/19/a-public-health-and-healthcare-spending-time-bomb-hepatitis-c/ on an assessment performed by the UK’s National Institute for Health and Clinical Excellence.
[206] Josiah D. Rich, Scott A. Allen, and Brie A. Williams, “Responding to Hepatitis C through the Criminal Justice System,” New England Journal of Medicine 370, pp. 1871-1874, http://www.nejm.org/doi/full/10.1056/NEJMp1311941.
[207] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 146.
[208] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 5.
[209] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 146.
[210] See WHO, Guidelines to Develop measures to combat counterfeit drugs, WHO/EDM/QSM 99.1 (1999),
http://whqlibdoc.who.int/hq/1999/WHO_EDM_QSM_99.1.pdf.
[211] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 146.
[212] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 5.
[213] Ellen ’t Hoen, “Turning the Tide: The WTO Doha Declaration on TRIPS & Public Health,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 31.
[214] WHO, “Health Topics: Essential Medicines,” http://www.who.int/topics/essential_medicines/en/, accessed on January 25, 2017.
[215] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 146.
[216] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 146.
[217] Ibid., p. 147.
[218] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 5.
[219] Ibid.
[220] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 147.
[221] Ibid.
[222] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 6.
[223] Ibid.
[224] Frederick M. Abbot, “Compulsory Licensing for Public Health Needs: The TRIPS Agenda at the WTO after the Doha Declaration on Public Health” (Quaker United Nationals Office, Geneva: February 2002), 49, www.quno.org.
[225] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 148.
[226] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 6.
[227] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 148.
[228] “Glossary” in High-Level Panel on Access to Health Technologies, Report of the United Nations Secretary-General’s High-Level Panel on Access to Medicines: Promoting Innovations and Access to Health Technologies (Geneva: UNHLP, September 2016), https://static1.squarespace.com/static/562094dee4b0d00c1a3ef761/t/57d9c6ebf5e231b2f02cd3d4/1473890031320/UNSG+HLP+Report+FINAL+12+Sept+2016.pdf, p. 6.
[229] Ellen ’t Hoen, “Annex 4: Glossary,” in Private Patents and Public Health: Changing Intellectual Property Rules for Access to Medicines (The Netherlands: Health Action International, 2016), http://accesstomedicines.org/wp-content/uploads/private-patents-and-public-health.pdf, p. 148.
[230] World Health Organization, “About WHO” fact sheet, http://www.who.int/about/what-we-do/en/.
[231] World Intellectual Property Organization, “Inside WIPO” fact sheet, http://www.wipo.int/about-wipo/en/.
[232] World Trade Organization, “The WTO” fact sheet, https://www.wto.org/english/thewto_e/thewto_e.htm.